Nearly 4 million people in the U.S. paid a visit to their physicians for "ankle symptoms" in 2004, according to figures cited by the American Academy of Orthopaedic Surgeons (AAOS). These symptoms can range from the commonplace ankle sprain to more serious foot fractures.
Of course, pinpointing ankle disorders caused by trauma or injury may be fairly simple, but what about asymptomatic ankles with anatomic variants? Could these structural idiosyncrasies make people more susceptible to ankle problems? And are there particular imaging anatomic hallmarks that clinicians should watch out for in the asymptomatic ankle? Yes, according to two studies out of Switzerland.
In the first study, Dr. Nadja Saupe and colleagues, from the Orthopedic University Hospital Balgrist and the Institute for Biostatistics in Zurich, looked at the anatomic variants that can lead to peroneal tendon disorders. They included the shape of the fibular groove, the size of peroneal eminences, and the position of the musculotendinous junction.
For their research, Saupe's group enrolled 65 volunteers (median age 45) with no trauma in the ankles over the last two years. These subjects underwent imaging on a 1.5-tesla system (Symphony, Siemens Medical Solutions, Erlangen, Germany). The protocol included T1-weighted spin-echo and T2-weighted fast spin-echo (FSE) imaging in the coronal plane, as well as FSE short inversion time inversion-recovery in the sagittal plane.
The images were reviewed by Saupe and co-authors Drs. Bernard Mengiardi and Marco Zanetti in consensus. They assessed for the following:
- Presence of an accessory peroneus quartus muscle
- Presence of prominences on the lateral aspect of the calcaneus
- Shape of retromalleolar fibular
- Presence of low-lying peroneus brevis muscle belly
- Position of peroneal tendons
They found that 17% of the volunteers had a peroneus quartus muscle, and that in the majority of cases (91%), the tendon inserted at the calcaneus as a peroneocalcaneus externum muscle. All of the subjects had a retrotrochlear eminence (100%), while a little over half (55%) had a peroneal tubercle. There were more instances of a flat retromalleolar fibular groove (43%) than a concave one (28%) or a convex one (18%).
In 85% of the volunteers, the peroneal tendons were centered.
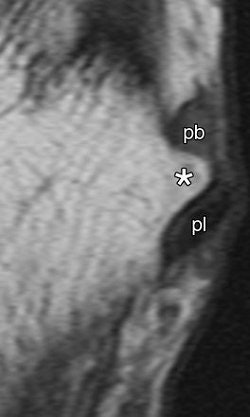 |
| Enlarged peroneal tubercle. T1-weighted MR images in (above) transverse oblique (45° between coronal and transverse planes, 572/14) and (below) coronal (572/14) planes show enlarged peroneal tubercle (*) in 60-year-old male asymptomatic volunteer. pb = peroneus brevis tendon, pl = peroneus longus tendon. |
 |
| Figure 3ab, Saupe N, Mengiardi B, Pfirmann C, Vienne P, et al. "Anatomic Variants Associated with Peroneal Tendon Disorders: MR Imaging Findings in Volunteers with Asymptomatic Ankles". Radiology 2007; 242(2): 509-517. |
"The median size of the peroneal tubercles was 2.6 mm on transverse oblique T1-weighted images and 2.9 mm on transverse T2-weighted images," the authors wrote. "The mean angle between the plantar fascia and the longitudinal axis of the tibia was 98˚" (Radiology, February 2007, Vol. 242:2, pp. 509-517).
The authors offered the following tips for imaging peroneal tendons:
- Look for a fat plane to distinguish the peroneus quartus muscle from a low-lying peroneus brevis muscle belly.
- The term "enlarged peroneal tubercule" and "enlarged retrotrochlear eminence" should only apply to structures of more than 5 mm.
- A low-lying peroneus brevis muscle belly requires muscle extension of more than 15 mm distal to the fibular tip
MCL complex
In the second paper, Mengiardi led a study on the medial collateral ligament (MCL) complex of the ankle, again focusing on asymptomatic subjects. Their goal was to assess the MR characteristics of the various MCL components: tibiospring ligament (TSL), the tibionavicular ligament (TNL), tibiotalar ligament (TTL), and the tibiocalcaneal ligament (TCL).
"The MCL complex is an important stabilizer not only against valgus forces but also against anterior and lateral talar excursion, as well as rotatory forces," wrote Mengiardi and colleagues. "Injuries of the MCL complex account for approximately 15% of ligamentous ankle trauma" (Radiology, March 2007, Vol. 242:3, pp. 817-824).
Previous MR studies of the MCL have relied on low-field-strength magnets and without spin-echo sequences, they added. For the current study, 56 asymptomatic volunteers (mean age 40.7) underwent imaging on a 1.5-tesla unit. The protocol included T1-weighted spin-echo images in the coronal, transverse oblique plane, and sagittal plane. A FSE short inversion time inversion-recovery sequence was also done in the sagittal plane.
The anterior and posterior TTLs from the deep ligaments, as well as the superficial layer of the TNL, TSL, and TCL, were defined on MR images. The thickness of the ligaments was measured.
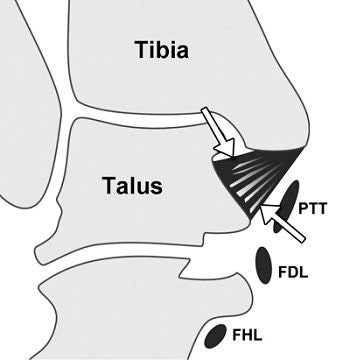 |
| Posterior TTL (posterior portion of the deep layer of the MCL complex) in asymptomatic 28-year-old woman. Above, corresponding drawing. Middle, T1-weighted coronal MR image (572/14). Below, T2-weighted coronal MR image (4130/86). The posterior TTL (arrows) originates from the upper segment of the posterior surface of the anterior colliculus, the intercollicular groove, and the anterior surface of the posterior colliculus. The fibers insert onto the medial surface of the talus. A typical striated appearance is seen on both T1- and T2-weighted images. |
 |
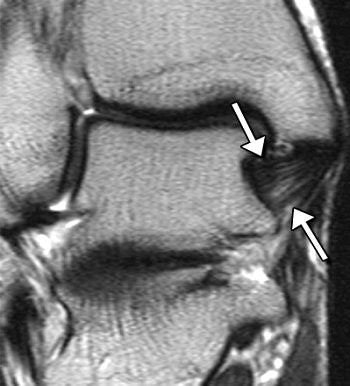 |
| Figure 3abc. Mengiardi B, Pfirmann C, Vienne P, Hodler J, et al. "Medical Collateral Ligament Complex of the Ankle: MR Appearance in Asymptomatic Subjects." Radiology 2007; 242(3): 817-824. |
According to the results, the anterior TTL, posterior TTL, TNL, TSL, and TCL were best seen on the coronal images. An inhomogenous pattern of the anterior TTL on T1-weighted images was seen in 21% of the subjects younger than 45 years and in 67% of those over age 45.
For the posterior TTL, the signal-intensity pattern was striated in 89% of the volunteers. It was also broader distally and had well-delineated borders. The authors suggested that the absence of striation in younger patients could be taken as a sign of possible TTL abnormality.
On T2-weighted images, the TSL had low signal intensity with a homogenous signal intensity pattern. For the TCL, the signal intensity was intermediate on T1-weighted images. The posterior TTL had a mean thickness of 8.2 mm, while the TCL had a mean thickness of 1.2 mm.
"In our study … the anterior TTL and TNL were seen in 55% of the ankles," the group wrote. "We assume that the limited visibility of the TNL … is at least in part explained by the oblique course of this ligament."
Because variable signal intensity for the anterior TTL, TNL and TSL was seen for older patients, Mengiardi's group cautioned against using signal intensity as an indication of ligamentous abnormalities.
A deeper understanding of the MCL remains important, as the most commonly injured ligaments are the TNL and TSL, resulting in ankle instability that can lead to proximal tears, distal tears, or avulsion, according to the authors.
By Shalmali Pal
AuntMinnie.com staff writer
March 16, 2007
Related Reading
Older men and women share similar risk of repeat fractures, January 24, 2007
High signal on T2 MR warns of poor healing after Achilles tendon repair, December 22, 2006
US overcomes x-ray's limits in pediatric ankle fractures, January 23, 2006
Copyright © 2007 AuntMinnie.com