Combining MR spectroscopy with T2-weighted MR imaging "significantly improves" the diagnostic accuracy of endorectal MRI to detect locally recurrent prostate cancer after external-beam radiation therapy, according to a study in the August issue of Radiology.
Researchers from the University of California, San Francisco (UCSF) concluded that the additional information may help advise patients about subsequent clinical evaluation, and help clinicians select patients for whom targeted prostateside biopsy is appropriate for confirming the disease (Radiology, Vol. 256:2, pp. 485-492).
Lead study author is Antonio Westphalen, MD, from UCSF's departments of radiology and biomedical imaging.
MR spectroscopy benefit
While endorectal MRI with T2-weighted sequences has become a reliable modality for the local detection and characterization of prostate cancer, the study authors noted that previous research has found T2-weighted MRI of the irradiated prostate may be limited by the post-treatment loss of zonal anatomy; diffuse low T2 signal may hinder tumor detection.
"As a result, MR spectroscopic imaging, a technique that enables the detection of abnormal metabolism rather than abnormal anatomy, has been investigated in this setting and yielded promising results in earlier studies," the authors wrote.
The retrospective study reviewed UCSF medical and radiologic databases between February 1999 and February 2008 and found 64 men with confirmed cases of prostate cancer. All 64 patients had received 1.5-tesla endorectal MRI, MR spectroscopy, and transrectal ultrasonographically guided biopsy for suspected local recurrence of prostate cancer after external-beam radiation therapy. Thirty-three patients also had received androgen therapy.
MRI exams were performed on a 1.5-tesla whole-body system (Signa, GE Healthcare, Chalfont St. Giles, U.K.). Patients were imaged with a body coil and a pelvic phased-array coil (GE) in combination with an expandable endorectal coil (Medrad, Warrendale, PA).
One experienced radiologist reviewed all MR images, while one experienced spectroscopist independently reviewed all MR spectroscopic data. Both specialists judged whether recurrent cancer was present or absent in the left and right sides of the prostate.
The researchers also calculated the receiver operating characteristic (ROC) curves for T2-weighted MRI alone and T2-weighted MRI with MR spectroscopy. The ROC curves were calculated by combining sensitivity and specificity results and using biopsy results as the reference standard.
Recurrent cancer
Recurrent prostate cancer was identified at biopsy in 37 (58%) of the 64 men, with unilateral recurrence in 28 patients, bilateral recurrence in nine patients, and a total of 46 affected prostate sides.
In the analysis, researchers determined that was a "significant difference" between ROC values for T2-weighted MR imaging alone (0.67) and ROC values for both T2-weighted MR imaging and MR spectroscopy (0.79).
The combination of MR spectroscopy and T2-weighted MRI also produced more true-positive results (59%) than T2-weighted MR imaging alone (41%), with no significant difference in the number of false-positive results. There were eight false positives (10%) with the combination of MR spectroscopy and T2-weighted MRI, compared with six false positives (7%) with T2-weighted MRI alone.
In addition, 14 prostate sides were incorrectly classified as negative for cancer with combined T2-weighted MRI and MR spectroscopy, while the diagnosis of recurrent disease was missed in eight patients with the combined technique.
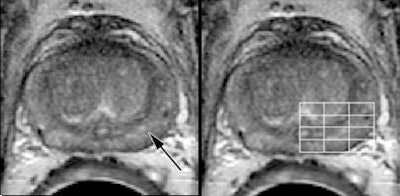 |
| A 60-year-old patient with biopsy-proven recurrent prostate cancer in the left side of prostate. Axial T2-weighted MR image (left) shows findings consistent with post-treatment changes (arrow). However, MR spectroscopic image (right) shows areas of malignant metabolism (line grid). Images courtesy of Radiology. |
The results of secondary analyses to compare the modalities in the subgroups of patients who did and did not undergo additional treatment with androgen deprivation therapy showed significantly different ROC values for T2-weighted MR imaging alone compared to T2-weighted MR imaging and MR spectroscopic imaging.
Secondary analyses
Among the patients who received prior androgen deprivation therapy, the ROC values were 0.69 for T2-weighted MRI and 0.83 for T2-weighted MRI and MR spectroscopy. For the patients who did not receive androgen deprivation therapy, the ROC values were 0.65 for T2-weighted MRI, compared with 0.76 for T2-weighted MRI and MR spectroscopy.
The authors noted several study limitations, including the retrospective single-institution approach, which could lead to selection bias, and that the results "may not be generalizable, as imaging acquisitions and interpretation expertise vary across institutions, particularly with MR spectroscopy."
The study also did not include a second reader for either the T2-weighted MRI or MR spectroscopic images, so researchers could not assess interreader variability.
Still, the authors had enough evidence to conclude that the combination of MR spectroscopy and T2-weighted MRI "significantly improves the detection of locally recurrent prostate cancer after definitive external-beam radiation therapy."
By Wayne Forrest
AuntMinnie.com staff writer
August 4, 2010
Related Reading
ARRS: MRI detects prostate cancer spread, April 28, 2009
MRI/MR spectroscopy falls short for prostate cancer, April 23, 2009
Longer hormone therapy may improve outcomes in advanced prostate cancer, April 15, 2009
SBRT for early prostate cancer shows promising interim results, April 9, 2009
No benefit seen with adjuvant radiotherapy after radical prostatectomy, March 25, 2009
Copyright © 2010 AuntMinnie.com