Squamous carcinoma of the penis is very rare in the U.S. The treatment tends to be a partial or total penectomy, often because urologists don't know that radiation therapy may be just as effective.
Instead, interstitial brachytherapy or external-beam radiation therapy should be considered as a treatment for penile cancer that manifests itself as a small-sized tumor. Even with extensive or advanced primary tumors, radiotherapeutic options should be considered before resorting to penectomy, according to research published online in the July 18 edition of World Journal of Urology.
In the study, a research team led by Dr. Juanita Crook, professor of radiation oncology at the University of Toronto and radiation oncologist at Princess Margaret Hospital in Toronto, described their success in using radiation therapy to treat penile cancer over a 19-year period at Princess Margaret Hospital and Ottawa Regional Cancer Centre.
A rare disease
Penile cancer represents less than 1% of male cancers, and the American Cancer Society (ACS) reports that 1,280 new cases were reported in 2007. With North America and Europe combined, it is estimated that 1 in 100,000 men get the disease.
New cases and deaths from penile cancer, U.S.
|
||||||||||||||||||||||||
| Statistics courtesy of the American Cancer Society. |
The vast majority of these men are not circumcised. Although a scientific correlation has not been proven, having a foreskin is a known risk factor for penile cancer, according to experts.
Penile cancer becomes evident as a painless ulcer or sore on the glans penis underneath the foreskin that does not heal. The majority of patients are over 50 years of age.
Interstitial brachytherapy
The two main forms of nonsurgical treatment for penile cancer are brachytherapy and external-beam radiation therapy.
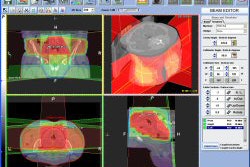
Penile brachytherapy generally delivers treatment to the full thickness of the penis using two or three parallel planes of needles. Intersource and interplane spacing should be equal, ranging from 12-18 mm, positioned to avoid the urethra and to ensure that the entire tumor and desired margin are within the high-dose volume.
The only significant predictor of local failure is needle spacing. For every unit increase in spacing there was a 52% reduction in the risk of local recurrence, according to the study.
Crook and colleagues noted that patients tolerate brachytherapy well. The patient is catheterized and remains in bed for the 4-5 days of treatment.
Of the patients, 85% had stage T1 and T2 tumors. Tumor size ranged up to 5 cm, the authors reported, with 30% under 2 cm, 32% at 2-3 cm, and 38% greater than 3 cm. Patients ranged in age from 22 to 93 years, with a mean age of 60.
The researchers reported a good success rate with brachytherapy. Of the 67 men treated between September 1989 and December 2007, 87% had no recurrence locally for five years, and 72% had no recurrence at 10 years. Only 12% of the patients required some form of surgery in the first five years. An additional 21% required surgery between five and 10 years later.
Conventional radiation therapy
The other treatment approach, external-beam radiation therapy, does not require the technical skill that brachytherapy does. It delivers a homogeneous dose and is widely available at treatment centers.
The penis is encased in a wax or Perspex block, or it is positioned in a water bath. A water bath provides the least discomfort for a patient during a protracted course of radiotherapy. Doses range from 60 Gy in 25 fractions over five weeks to 74 Gy in 37 fractions over 7.5 weeks.
External radiation therapy is not as successful at local control as brachytherapy, with penile preservation rates falling to 36%-66% at five years, Crook and colleagues reported.
In an independent commentary on the Canadian team's results, Dr. Anthony Zietman, professor of radiation oncology at Harvard Medical School and a specialist in urologic oncology at Massachusetts General Hospital, both in Boston, explained the lower success rate of radiation therapy. He said that external radiation therapy is used with larger and/or deeper tumors, which tend to be more aggressive than smaller ones.
Changing management?
Could the Crook team's results lead to a change in the way penile cancer is managed in North America? Many urologists in Canada and the U.S. don't currently suggest radiotherapy as an alternative to surgery, according to Crook -- and echoed by Zietman.
"The convention in the U.S. is to perform surgery first, followed by radiation if there are complications," Zietman said. "The emphasis in Europe is to spare the penis. The experts in Europe do radiation first followed by surgery if there are complications."
While penile cancer has a tendency to spread quite early, Zietman stated that he and his colleagues have not seen any evidence that surgery or radiation therapy is a more effective treatment option than the other.
"Surgery should be the treatment of last resort," Zietman said. "I know of patients who have committed suicide after a penectomy. The surgery may be successful, but the psychological effects are devastating."
By Cynthia Keen
AuntMinnie.com staff writer
September 16, 2008
Copyright © 2008 AuntMinnie.com