CHICAGO - Researchers suggest they have a better option than mastectomy and breast reconstruction for women with breast augmentation implants who have been diagnosed with early-stage breast cancer.
The option is a five-day course of brachytherapy in which radioactive seeds are precisely placed in a series of catheters utilizing CT technology.
"We have had no recurrences after a median of two years following treatment, and the cosmetic outcomes have been judged excellent in more than 90% of the women," said Dr. Robert Kuske, director of the freestanding Advanced Providers of Breast Irradiation (APBI) clinic in Scottsdale, AZ, at the 2008 RSNA conference.
Kuske said breast augmentation is considered a contraindication for whole-breast radiation because it is associated with an increased risk of capsular contracture, resulting in pain and poor cosmetics.
According to Kuske, the problem is growing rapidly in the U.S. where breast augmentation surgery is being performed 350,000 times a year -- nearly nine times more frequently than in 1991.
"Having a breast implant does not increase a woman's risk of developing breast cancer," Kuske said, "but one in eight of these women will eventually develop breast cancer, similar to the rest of the population. That means about 49,000 of these women will have to be treated for breast cancer in their lifetimes."
"By their nature, these women have demonstrated a personal priority on appearance and cosmetics, but currently the accepted treatment for breast cancer in patients with implant augmentation is skin-sparing mastectomy with axillary dissection and implant exchange," he said.
Even though these women would be eligible for breast-conserving therapy, their options are limited because whole-breast radiation results in capsular contraction about 50% of the time, Kuske noted. "Since brachytherapy exposes only a small portion of the surface area of the implant to radiation, it is possible that the rate of capsular contracture might be reduced by partial-breast irradiation with brachytherapy," he said.
In a series of 70 women who underwent the brachytherapy procedure, "there was not a single case of capsular contracture, and cosmetic results were excellent in 91% of patients and good -- meaning slight breast asymmetry -- in 9% of patients," Kuske said. No women had fair or poor results in what he said was the first study of image-guided brachytherapy in women with augmentation.
He also reported that no breast cancer recurrence was observed in up to 26 months of follow-up. Kuske said he was confident that the treatment would be effective, "because this technique has been studied for 18 years in women who don't have breast augmentation, and in those studies the recurrence rate with brachytherapy is about 5%, which is comparable to the rate with whole-breast irradiation."
Dr. Joseph Tashjian, president of St. Paul Radiology in St. Paul, MN, said the data from the studies of brachytherapy in women without implants did provide evidence of the safety of the procedure.
Image-guided brachytherapy was, Tashjian said, "a very good technique, but the real benefit is five days versus more than six weeks of radiation. That is a huge benefit."
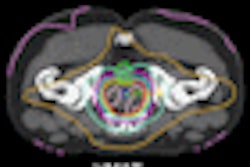
In Kuske's procedure, the patients underwent lumpectomy to remove lesions less than 3 cm; they had fewer than four cases of lymph node involvement. The mean age of the women was 50 years. Following surgery, Kuske used a template made by Nucletron (Veenendaal, Netherlands) to compress the breast tissue above the implant. He helped develop the template.
This same template is used for mammograms in women who have implants. The operator pulls the breast tissue out from the implant and then compresses the tissue between the templates. The breast is then imaged with CT.
Using the CT image to guide the process, the radiologist then inserts brachytherapy capsules into the breast through catheters inserted into a series of predrilled holes that are used to guide the needles and "avoid puncturing the implant."
Kuske said that he has not had a single capsule puncture using this procedure. The dose prescription was 34 Gy in 10 twice-daily fractions with high dose rate iridium-192, and the treatments were separated by at least six hours.
By Edward Susman
AuntMinnie.com contributing writer
December 1, 2008
Copyright © 2008 AuntMinnie.com