“Living” and “viable” should be avoided in first-trimester ultrasound lexicon when imaging pregnant women, according to new guidelines introduced August 27 by the Society of Radiologists in Ultrasound (SRU), published in Radiology.
In what the RSNA is calling a first, the lexicon developed by a multisociety panel addresses terms frequently used in first-trimester ultrasound reports, such as “ectopic pregnancy,” “heartbeat,” “living,” and “viable.”
“Our goal was to recommend clear, specific, scientifically based, and medically appropriate terminology that communicates clearly across disciplines, minimizes bias and harm, and respects patient preferences,” stated senior author Lori Strachowski, MD, from the University of California, San Francisco (UCSF), in a news release.
Medical professionals, including radiologists, continue to navigate a murky legal landscape when it comes to fetal health services since the overturning of Roe v. Wade with the 2022 U.S. Supreme Court ruling on Dobbs v. Jackson Women's Health Organization.
Varied and changing state-level policies have added to the confusion about how to best go about imaging pregnant women as well as women who may not know if they’re pregnant but decline testing.
Additionally, legal and political organizations could use ultrasound findings and specific language in the medical record to negatively affect the physician-patient relationship as well as criminalize patients and practitioners.
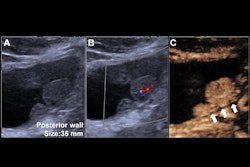
 An intradecidual sign depicts transvaginal sagittal grayscale ultrasound imaging in a 34-year-old pregnant patient, which shows a 4-mm empty gestational sac (solid arrow) in the anterior endometrium. The location of the sac to one side of the central hyperechoic line (dotted arrows) representing the opposed innermost layers of decidualized endometrium confirms it is within the endometrium and not the endometrial cavity, hence the name intradecidual sign. This sign is helpful when seen to diagnose a probable intrauterine pregnancy before visualization of the yolk sac. Three days later, the yolk sac was visualized (not shown), allowing for the diagnosis of a definite intrauterine pregnancy.RSNA
An intradecidual sign depicts transvaginal sagittal grayscale ultrasound imaging in a 34-year-old pregnant patient, which shows a 4-mm empty gestational sac (solid arrow) in the anterior endometrium. The location of the sac to one side of the central hyperechoic line (dotted arrows) representing the opposed innermost layers of decidualized endometrium confirms it is within the endometrium and not the endometrial cavity, hence the name intradecidual sign. This sign is helpful when seen to diagnose a probable intrauterine pregnancy before visualization of the yolk sac. Three days later, the yolk sac was visualized (not shown), allowing for the diagnosis of a definite intrauterine pregnancy.RSNA
The SRU sought to minimize preventable adverse outcomes and protect patients and clinicians by convening a multi-society panel of experts to develop a lexicon for first-trimester ultrasound reports. The panel identified terms that are clear, specific, scientifically based, and medically appropriate, as well as acceptable to imagers, clinicians, and patients. Additionally, it wanted to minimize bias and harm with the new lexicon.
“The scope of this lexicon is limited to terms generally unique to and frequently encountered during the first trimester,” the SRU added.
Key recommendations from the panel include the following:
- "Early pregnancy loss" should replace "pregnancy failure" and should be used with the following modifiers: concerning for, diagnostic of, in progress, incomplete, and completed.
- "Cardiac activity" should be used instead of "heart motion" in the first trimester, and the terms "live," "living,” and "viable" should also be avoided.
- "Ectopic pregnancy" should be defined as an abnormal pregnancy implantation and includes both extrauterine and intrauterine sites, such as the cervix or cesarean scar.
The lexicon highlights that all ectopic pregnancies carry an increased risk of maternal morbidity and mortality. Additionally, avoiding the use of “pregnancy failure” considers patient preferences and addresses guilt among pregnant women, the SRU stated.
In an accompanying editorial, Leslie Scoutt, MD, from Yale School of Medicine in New Haven, CT, and Mary Norton, MD, from UCSF applauded the initiative. They added that they hope the lexicon is “widely adopted and integrated into clinical pathways by all healthcare systems and subspecialties.”
“As healthcare systems continue to grow and become more complex, as imaging becomes increasingly multidisciplinary, and as the imaging report becomes more patient-centric, it is critical that healthcare providers use universal terminology to avoid miscommunication and thus inappropriate patient care as well as language that fosters patient well-being,” Scoutt and Norton wrote.
The full recommendations can be found here.