Contrast-enhanced mammography (CEM) can accurately identify pathologic nipple involvement in breast cancer patients, suggest findings published November 4 in Radiology.
A team led by Andrea Cozzi, MD, PhD, from the Imaging Institute of Southern Switzerland in Lugano found that CEM achieved high specificity and positive predictive value (PPV) for ruling in nipple involvement. It also reported specific imaging features tied to pathologic nipple involvement.
“As CEM implementation is growing, especially in the preoperative setting, our results show that preoperative CEM … can preclude attempts at nipple-sparing surgeries that would then require the transition to more aggressive surgery,” the Cozzi team wrote.
CEM is conditionally recommended for diagnostic workup in the European Guidelines framework and in the American College of Radiology (ACR) Appropriateness Criteria. CEM in prior studies has shown accuracy that is on par with that of breast MRI for lesion detection. However, the team noted a lack of data on CEM’s diagnostic accuracy for assessing pathologic nipple involvement.
Cozzi and colleagues studied CEM’s potential to consistently identify the presence of tumor involvement of the nipple. They used surgical pathologic evaluation as the reference standard and evaluated associations between several CEM features and pathologic nipple involvement.
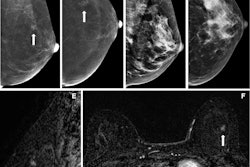
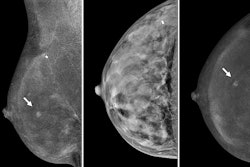
 Preoperative CEM images in a 73-year-old female patient show true-positive findings of a nonluminal ERBB2-positive (formerly HER2 or HER2/neu) grade 3 invasive carcinoma of no specific type, with a spiculated mass with high conspicuity heterogeneous mass enhancement in the posterior third of the right upper outer quadrant. An area of high conspicuity clumped nonmass enhancement with associated microcalcifications (craniocaudal view of low-energy images in A; craniocaudal view of recombined images in B) extended from the mass to the nipple-areolar complex (minimum enhancement-to-nipple distance on the craniocaudal view, 0 mm), which on a (C) photomicrograph (hematoxylin-eosin stain at ×50 magnification) was completely infiltrated by malignant epithelial cells with diffuse desmoplastic stromal reaction, consistent with tumor involvement. Three residual normal ducts (arrows in C) were still present. Aside from the continuity of the nonmass enhancement with the nipple-areolar complex, other findings at CEM that were consistent with pathologic nipple involvement were the presence of an inverted nipple type and of nipple retraction (A, B), periareolar skin thickening (arrow in A), and disruption of the superficial linear enhancement (arrowheads in B).RSNA
Preoperative CEM images in a 73-year-old female patient show true-positive findings of a nonluminal ERBB2-positive (formerly HER2 or HER2/neu) grade 3 invasive carcinoma of no specific type, with a spiculated mass with high conspicuity heterogeneous mass enhancement in the posterior third of the right upper outer quadrant. An area of high conspicuity clumped nonmass enhancement with associated microcalcifications (craniocaudal view of low-energy images in A; craniocaudal view of recombined images in B) extended from the mass to the nipple-areolar complex (minimum enhancement-to-nipple distance on the craniocaudal view, 0 mm), which on a (C) photomicrograph (hematoxylin-eosin stain at ×50 magnification) was completely infiltrated by malignant epithelial cells with diffuse desmoplastic stromal reaction, consistent with tumor involvement. Three residual normal ducts (arrows in C) were still present. Aside from the continuity of the nonmass enhancement with the nipple-areolar complex, other findings at CEM that were consistent with pathologic nipple involvement were the presence of an inverted nipple type and of nipple retraction (A, B), periareolar skin thickening (arrow in A), and disruption of the superficial linear enhancement (arrowheads in B).RSNA
The study included data collected between 2016 and 2023 from 530 women with biopsy-proven breast cancer. The women had their cancers, 558 in total, treated via primary surgery, and they underwent preoperative CEM at five referral centers.
The team reported pathologic nipple involvement in 147 of the total cancer cases (26.3%). CEM achieved an average specificity of 95.1% and an average PPV of 83.5% for the five referral centers. The modality also demonstrated an average positive likelihood ratio of 14.1.
The researchers also reported the following features that are significantly associated with pathologic nipple involvement: periareolar skin thickening (odds ratio [OR], 3.8; p < 0.001), disrupted superficial linear enhancement (OR, 3.0; p = 0.01), and nipple retraction (OR, 2.2; p = 0.03).
However, 1-mm increases in the minimum enhancement-to-nipple distance led to significantly lower odds (OR, 0.94; p < 0.001) of nipple involvement.
Finally, a cutoff of 9.5 mm best predicted pathologic nipple involvement for the minimum enhancement-to-nipple distance, with a Youden index value of 0.53. This finding is similar to the 11.5-mm cutoff reported for MRI.
“Notably, both of these cutoff values are in accordance with reports indicating that the commonly cited 20-mm threshold could be lowered without compromising oncological safety,” the researchers wrote.
Cozzi and colleagues called for more studies to determine how much CEM features and the minimum enhancement-to-nipple distance can define CEM’s accuracy for ruling in pathologic nipple involvement.
Read the full study here.