Given the low positive predictive value of the usual six-month follow-up, a one-year follow-up of BI-RADS 3 mammograms may be more appropriate, according to an analysis of data from the U.S. Women’s Health Initiative (WHI).
Dr. Shagufta Yasmeen from the University of California, Davis and colleagues looked at 2,957 mammograms for which a short-interval follow-up was recommended. Their concern was that "early recall for follow-up testing on screening mammography causes anxiety, psychological morbidity, and increased healthcare utilization in the year after a false-positive mammogram is reported (Journal of the National Cancer Institute, March 19, 2003, Vol. 95:6, pp. 429-436).
Yasmeen’s co-authors are from the Fred Hutchinson Cancer Research Center in Seattle; the Harbor-University of California at Los Angeles Research and Education Institute in Torrance; the State University of New York at Stony Brook; and Wayne State University in Detroit.
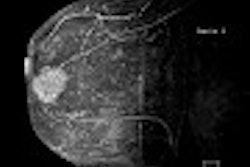
"BI-RADS category 3 is applied to mammograms that show abnormalities that have a very high probability of being benign," they wrote. "Such abnormalities are not expected to change over the follow-up interval, but the radiologist would prefer to establish their stability."
For this analysis, women in the WHI clinical trial arms who had a baseline screening mammogram, and two-year follow-up data, were included (58,408 women). The WHI is a prospective study of 161,860 postmenopausal women who enrolled from 1993 to 1999 at 40 U.S. clinical centers. Based on WHI forms, potential breast cancer risk factors included age, body mass index, hip-to-waist ratio, family history, and age at menopause.
Out of the 58,408 women, 5% had received recommendations for short-interval follow-up. "Negative and benign mammograms were considered false negatives if the participants were diagnosed with breast cancer within the subsequent two years. A mammogram with a recommendation for short-interval follow-up was considered a false positive if the participant was found not to have breast cancer within two years of follow-up," the authors explained.
According to the results, the incidence of breast cancer for these women was 1.02% at two years after the baseline mammogram. For women with baseline mammograms described as negative, the breast cancer incidences were 0.6%; for benign mammograms it was 0.5%. The tumor size at diagnosis ranged from 8-20 mm.
The likelihood ratio for breast cancer after a recommendation for short-interval follow-up on a subsequent mammogram was 2.20 (95% confidence interval). "Of the 308 cases of breast cancer that were newly diagnosed within two years after the baseline mammogram, only 10% occurred in women…with short-term follow-up," they wrote.
Women who had recommendations for short-term follow-up generally had higher mean body mass index and a higher mean hip-to-waist ratio, the group found. However, a family history of breast cancer and age at menopause were not considered significant correlates.
The prevalence of short-interval follow-up recommendations across the 40 centers ranged from 1.2% to 9.8%. The authors acknowledged that the quality of mammography varied across the country and that the reliability of interpretations may be an issue because, in most cases, only one radiologist read the images.
"WHI does not collect information about where the mammogram was done, who read the mammogram ( faculty, resident, radiologists who specialize in reading the mammograms and single or double reading, etc.)," Yasmeen explained in an email to AuntMinnie.com. "Our generalizable study represents the variability in the practice patterns among the radiologists and an important finding on higher prevalence of (5.2%) from our study results compared to the bench mark of 1.2%"
However, "given the fact that recommendation for short-interval follow-up may account for over 50% of abnormal screening mammograms, our results should stimulate re-examination of the criteria used to make this recommendation (that may) lead to more mammographic examinations, and, probably, more biopsies for changes that turn out to be benign."
By Shalmali PalAuntMinnie.com staff writer
March 21, 2003
Related Reading
Breast center enlists radiographers for first look at mammograms, March 11, 2003
RTs score well in breast imaging classification, January 22, 2003
Multiple-reading protocol bolsters interpretation for non-mammographers, September 6, 2002
Weight gain, waist-hip ratio identified as risk factors for breast cancer, June 1, 2002
CAD cuts false negatives, increases sensitivity of breast imaging, November 28, 2001
Copyright © 2003 AuntMinnie.com