Potential investigators for the American College of Radiology Imaging Network (ACRIN) 6666 breast ultrasound trial must continue to hone their skills in interpreting postoperative images, according to a presentation at the 2004 RSNA meeting in Chicago. The results of self-assessment quizzes indicate that readers have a difficult time distinguishing between cancer recurrence and postsurgical scarring.
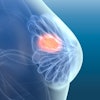
ACRIN 6666, which began enrolling women in March 2004, will include 2,808 women at 20 U.S. institutions to determine the exact role of ultrasound in those who are at high risk for breast cancer. The women will receive mammograms and physician-performed sonographic exams annually for three years. The study's primary aim is to evaluate the performance of whole-breast screening ultrasound combined with mammography, and compared to mammography alone.
"Breast cancer patients, diagnosed one year earlier, comprise perhaps the largest group of the enrollees to date," said Dr. Ellen Mendelson from the Feinberg School of Medicine at Northwestern University in Chicago. "Our purpose in this study was to ascertain the accuracy of potential investigators in differentiating scar and other post-treatment changes in breast cancer in mammograms and sonograms of the treated breast."
The 35 experienced breast imagers for this study also were tested on their ultrasound interpretation skills in another report, which was presented at RSNA by Mendelson's co-author, Dr. Wendie Berg, Ph.D.
For this particular study, the investigators were given quizzes using mammography and ultrasound cases that included masses and calcification. The quizzes were taken twice, before and after feedback. The readers were allowed to look at the patient's mammograms, but not simultaneously with the ultrasound images, Mendelson said.
The cases included cancers prior to breast carcinoma diagnoses, cases with benign findings, and cases of treated breast cancer, with and without recurring cancer. A set of 28 sonograms was presented to potential investigators, and included eight cancers and 20 benign cases. The set of 34 mammograms included 20 cancers and 14 benign cases, Mendelson said.
The investigators assigned each case a BI-RADS final assessment category with the correct answers supported by pathology, a four-year period of imaging stability, or a decrease in lesion size. Sensitivity and specificity were calculated for each reader; ROC curves were generated. The postsurgical performances of individual investigators, as well as the entire group, were compared to their scores for masses and calcifications prior to the cancer.
The results showed a significant drop in sensitivity for both mammography and ultrasound when responses for the treated breast were compared to images prior to diagnosis.
"For mammography, sensitivity dropped from 93% to 65%. For ultrasound, which also had high sensitivity for masses and calcifications prior to diagnoses, the drop was from 89% to a relatively poor 60% in the treated breast," Mendelson said. The Az for ultrasound was 0.65 and 0.77 for mammography. Specificity either remained the same or improved slightly in the treated breast (61% to 68% for ultrasound, 81% for mammography), but there was no obvious explanation for that shift, she added.
Mendelson highlighted some of the best and worst cases in the quiz set. All the cases were orthogonal views in the same region at the site of the tumor bed. The investigators easily identified architectural distortion at the site of the tumor incision as postsurgical and radiation changes. They also did well on identifying focally thickened skin with a tract extending from the skin down to the tumor bed, where the scalpel had excised the skin.
One problematic case involved a nodular area -- irregular in shape, microlobulated, indistinctly marginated, and containing mircocalcifications -- at the lumpectomy site. This could have been fat necrosis, but the majority of the investigators tagged it as suspected cancer, when it was actually recurrent invasive ductal carcinoma, Mendelson said.
Another case involved a mass-like finding and a focally thickened area forming a "V" at the skin. Finally, a case that truly confounded the investigators had a small nodular area adjacent to the lumpectomy site. Most of the investigators pegged it incorrectly as recurrent cancer.
"Ultrasound and mammographic appearances of breast cancer and post-treatment changes are similar, and will need to be distinguished by investigators surveying these conserved breasts," Mendelson concluded. "Changes after conservation are more difficult to assess in the unaltered breast, with significant drop in sensitivity for both mammography and ultrasound."
Feedback and discussion improved interpretive performance, she added, and continued assessment quizzes may be beneficial in training potential investigators.
By Shalmali Pal
AuntMinnie.com staff writer
December 22, 2004
Related Reading
Breast imagers fare better with hands-on approach to screening ultrasound, December 17, 2004
ACRIN updates multiple breast cancer trials, April 15, 2004
Breast ultrasound experts share pearls and pitfalls, October 2, 2003
Copyright © 2004 AuntMinnie.com