It's no secret that PACS requires an extensive support system and a coordinated team in order to operate successfully. And there may be no more critical role than that of the PACS system administrator (SA). The scope of a PACS SA position crosses multiple arenas, and requires a well-managed team approach.
Successful performance of a PACS system requires the synergy of three main groups: information technology, biomedical engineering, and the technology's end users -- the radiologic technologists (RT), and radiologists. A PACS SA or analyst must serve as an interface between these entities to ensure smooth functioning of the system. Other players in the game include medical physicists and equipment vendors.
A PACS SA works with IT in areas such as maintenance, upgrades, and hardware and software changes. Biomedical engineering (BE) handles preventive maintenance and places great emphasis on monitor calibration. The PACS SA relies on the combined expertise of BE and the medical physicist to ensure that image viewing quality and integrity are not sacrificed in any way.
RTs rely on the PACS SA for hands-on system help and troubleshooting. The PACS SA also frequently interfaces with vendors regarding systems issues that cannot be resolved internally.
Requirements for success
What does it take to be an effective PACS SA? A background in computers, networking and system troubleshooting are a good basis to build upon. Some level of clinical expertise is also critical.
A PACS SA is responsible for bridging technology with clinical applications, and therefore needs to be familiar with terminology and RT techniques. A background in training would also be most helpful, as SAs also teach numerous people how to use the PACS system.
The SA must understand the HL7 (front-end) and DICOM (clinical) communication standards that support PACS. A comprehensive understanding of integration profiles as defined by the IHE (Integrating the Healthcare Enterprise) initiative is also important.
IHE profiles are sets of DICOM and HL7 messages, and include a specification on how to map specific attributes between the two standards. They link the two languages together, in pre-defined sets, for effective functioning and communication.
A PACS SA also needs to have good people skills. Interfacing with the supporting PACS teams requires effective communication, teaching, and troubleshooting capabilities. Working with myriad people across multiple platforms will put the SA in countless interactive situations. The ability to adapt to, and work with, many people will come in quite handy.
The scope of a PACS SA can vary greatly, with no two job descriptions across institutions exactly alike. Each hospital rests at a different place in their PACS implementation and system maturity.
In addition, the knowledge level of existing team players will play a critical role in any given PACS SA job description. History plays a key factor in defining this role as well; some facilities align their SA closely with IT while others find that their operation runs more smoothly with a close RT/SA relationship.
The PACS SA's key activities can be defined within the context of three broad areas: project management, system maintenance, and image management.
Project Management
The planning and implementation of a new PACS system can take anywhere from three to nine months, and involves many factors including training, equipment location, space, monitor placement, and even environmental factors such as power requirements (including backup and UPS), and air conditioning. Comprehensive coordination of a new PACS installation is an enormous undertaking.
Any PACS SA should understand the institution's workflow. Creating a map of the information flow will help define system placement, configuration, routing, testing, and maintenance. This map should include collection of patient information and the examination process. It ends with image viewing, storage, and the generation of diagnostic reports.
Post-installation management includes adding software upgrades, new modalities, workstations, interfaces, and users to the system. Successful management of these jobs involves the anticipation of cause-and-effect relationships.
For example, will an HL7 upgrade affect existing IHE profiles and therefore impact how patient demographics appear at a modality? Thorough testing as well as and coordinated scheduling of changes and upgrades is critical. Doing so will help eliminate the possibility of system problems.
Training and support are needed to ensure the smooth daily operation and management of a PACS. An SA will work with vendors to train users on new releases and upgrades, as well as develop materials for the staff.
Hardware and software issues, operator questions and errors, system bugs or failures, and emergency situations all require immediate support. The SA must provide access to an "on-call" system. Most support activities fall under system maintenance, the second key area of responsibility of a PACS SA.
System maintenance
A PACS SA is the first line of support for configuration management and control functions. This process includes, but is not limited to, managing DICOM application entity (AE) titles, as well as implementing and maintaining a configuration control board. The SA will also be responsible for performing preventive maintenance, general system maintenance, HIPAA compliance, modality acceptance testing, and interface testing.
Managing DICOM AE titles, which identify workstations, modalities, and archive locations for the purpose of DICOM communication, is essential for installing new equipment, as well as for hardware and software upgrades. Documenting and physically mapping the system prevents potential compatibility issues whenever systems changes are made, and is essential for proper software functionality.
Recording new and upgrade software releases goes hand-in-hand with this process. It’s important to know which devices run with which software for future upgrade purposes. Finally, hardware configuration and changes should be documented regularly.
The PACS network works in tandem with the radiology information system (RIS), and acquisition modalities. As such, it is important that the people managing these systems and devices communicate regularly.
These groups of people make up a "configuration control board," and are responsible for planning events that will collectively affect their system or device. A PACS SA should establish a control board and ensure its synergistic operation.
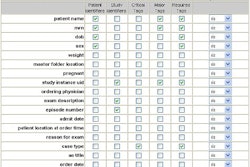
Preventive maintenance, which can be managed with a simple checklist, drastically reduces problems. This checklist could include such functions as monitoring image quality among modalities, workstations, and printers, and checking unresolved study queues.
Scheduling regular checks and system testing also improves reliability, and increases the ability to make system enhancements and improvements. A preventive maintenance schedule will grow and change with the system.
The SA will also need to keep a catalog of users, and assign appropriate security access, in line with the privacy and security provisions of the Health Insurance Portability and Accountability Act (HIPAA). Hospital employees need to be provided with varying degrees of access to imaging and patient information based upon their authorization level.
Documenting and tracking the distribution or disclosure of an image/patient information through audit trails can be considered part of the general system maintenance. In managing this responsibility, a PACS SA works closely with a hospital’s chief security officer or chief privacy officer to ensure HIPAA compliance.
Acceptance testing is performed with new equipment that is added to the system. The best way to execute acceptance testing is to maintain a "shadow system," which reflects the same characteristics as the main PACS, but operates in a "dummy" mode.
Testing the addition of a new modality, software upgrade, or hardware in this environment is very successful in identifying potential compatibility issues. In addition to physically testing compatibility, paper validation is very important. Reviewing the documents, features, and interface specifications provided with the upgrade or addition could potentially prevent compatibility issues.
When installing a new modality, the modality interface should be tested. At a minimum, patient demographics should be available through DICOM modality worklist support.
Image management
Proper acquisition of an image is the first step in achieving good image quality. The skill level of a RT can impact how the image appears. In addition, patient movement during an exam may also contribute to image "fuzziness."
Dust or scratches on the image plate can affect quality during computed radiography (CR) procedures. When troubleshooting an image quality issue, a PACS SA must consider all of these factors.
The computer monitor used at the viewing station bears perhaps the greatest impact on image quality. Image quality from one monitor to the next must be consistent, so that regardless of the viewing station, the image on screen represents the "real thing."
Monitor calibration using specialized tools ensures that monitor displays are corrected for any drifts or aging of the hardware. The DICOM standard, the American Association of Physicists in Medicine (AAPM), and most vendors specify calibration testing patterns and tools.
Test patterns also ensure that image quality is maintained at the output level, matching hard copy consistently. These tools are very helpful, and critical for a SA to ensure consistent image presentation.
Data integrity refers to the information stored in the so-called "image header." When correctly combined, an image properly shows and stores the corresponding patient demographics. When some element is missing -- usually part of the patient information, it could result in what most users refer to as a "broken study."
These errors can happen during an emergency exam or due to data input error. Whatever the case, broken studies must be resolved or placed in a temporary folder or holding area, otherwise, a queue forms at the PACS gateway and/or archive, and prevents images from being available for physician viewing. It's the SA's job to implement a process to handle broken studies and manage problems associated with them.
The need for data integrity also comes into play when merging and splitting studies. These processes are sometimes necessary when viewing a large portion of the body (merging images into a single study), or when multiple physicians need to view different parts of a large image set (splitting a series of images into multiple studies). Accession numbers assigned to each study component by the RIS assist in merging and splitting studies.
Short-term, mid-term, and long-term storage solutions are an essential part of any PACS. Immediate accessibility is typically achieved through the online access of a RAID storage system, which is also popular for short-term and mid-term image storage needs. An optical disc or tape jukebox is usually deployed to handle long-term storage -- typically for studies older than six months.
Images older than three years can be stored offline; a PACS SA should check for potential retrievals and "mount" the off-line media to allow the images to be available online.
The important and wide-ranging responsibilities associated with PACS administration clearly make it a varied and challenging career. Moreover, the rapid deployment of PACS networks is creating new opportunities for people with some of the interests and skills needed to do the job.
By Herman OosterwijkAuntMinnie.com contributing writer
April 10, 2003
Herman Oosterwijk is president of OTech, Inc., a Dallas-based healthcare technology consulting and training firm. OTech also provides books and e-learning courses for system administrators at www.otechimg.com.
Related Reading
Offsite ASP archive fulfills disaster-recovery, backup requirements, January 21, 2003
Clinical IS audits tune performance, productivity, October 3, 2002
Oversight committee, project management smoothes PACS operation, September 10, 2002
Image quality is still job one for PACS, August 31, 2001
Copyright © 2003 AuntMinnie.com