WASHINGTON, DC - Is the Centers for Medicare and Medicaid Services (CMS) more talk than substance on the issue of physicians making money from self-referrals and related imaging interpretation services?
While the agency has attempted to put safeguards in place, assorted delays and court action have stymied the progress of any significant regulatory actions to rein in physician self-referral.
Attorney Thomas Greeson, a partner at law firm Reed Smith of Falls Church, VA, offered his perspectives on the CMS during the opening day of the American Roentgen Ray Society (ARRS) annual meeting in Washington, DC. Greeson specializes in radiology-related regulatory matters.
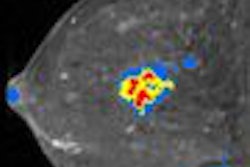
CMS is looking closely at rising costs for imaging services, in part because of the growth in diagnostic imaging and clinical applications over the last decade. MedPAC, an independent federal entity that advises the U.S. Congress on Medicare issues, reported to lawmakers in 2005 that imaging services represented the fastest-growing component of the Medicare Physician Fee Schedule (MPFS).
In addition, from 1999 to 2003, all physician services paid through the MPFS increased by 22%, while imaging services grew by 45%. MRI payments alone climbed 99% during that time.
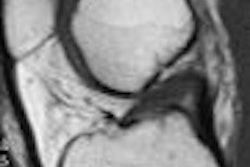
In-office imagingDriving the growth in imaging costs are specialists such as cardiologists, orthopedists, urologists, and oncologists who are buying their own equipment and performing in-office scans on their own patients.
What CMS is starting to focus on are fee-per-scan and equipment block-time "leasing" arrangements between specialists and outside imaging centers. Such arrangements have become very controversial and increasingly have been subject to investigation by law enforcement agencies, federal and state regulators, and local attorneys general.
"They are the kinds of arrangements that many policy makers have expressed concerns about," Greeson said. "There are situations where physicians don't own their own imaging facility and enter into a lease arrangement with an imaging center…. The physician bills the insurer for that service and pockets the difference between the purchase price and the price they bill the carrier."
Specifically, CMS is targeting independent diagnostic testing facilities (IDTFs). In November 2007, the agency proposed a set of new regulations for IDTFs and adopted performance standards extending the requirements for supervising physicians of IDTFs. Many of the changes went into effect on January 1.
Ambiguous standardsWhile the standards were "a bit ambiguous," Greeson believes, CMS in 2008 indicated that no physician can perform general supervision at more than three IDTF sites (although a radiologist can perform direct and personal supervision at more than three IDTFs). CMS also stipulated that a fixed-site, nonhospital-based IDTF may not share its practice location with another physician practice and may not lease or sublease its operations to another entity.
"And, if an IDTF is located inside a physician's office, (CMS) has allowed that physician's office a year to disentangle itself from that physical space-sharing arrangement," Greeson added. That space-sharing prohibition goes into effect on January 1, 2009.
The most significant CMS action, Greeson said, is in the "markup" of certain technical and professional component services. "CMS has said, 'The Stark rules will permit you to bill for self-referred imaging services, but we are taking away the profit from some of it,' " Greeson explained. "An anti-markup prohibition has been longstanding in the Medicare rules, but it has had a very narrow application until now."
In the final rule, CMS adopted a newly revised anti-markup rule that applies to technical-component services and purchased professional interpretation services.
Anti-markup rule"As adopted last fall, CMS recognized they should apply this anti-markup rule only to self-referring physicians," he said. "So, the trigger for this anti-markup rule is when a physician orders a diagnostic test and that service -- the technical component or the professional interpretation service -- is either purchased outright from an outside supplier or either the technical or professional component is performed outside the physician's office."
In January, CMS delayed implementation of the anti-markup rule to January 1, 2009, with one exception -- diagnostic tests that are performed for anatomical pathology by a centralized location that qualifies under Stark regulations.
CMS created the exemption in response to so-called "pod labs," which handle tests for referring physicians. "There could be as many as 20 or 30 individual, exclusive pods that were technically created for the purpose of allowing that referral to meet the centralized-location requirement for the Stark in-office ancillary services exception," Greeson said. "Clearly, it is a perfect example of how the delivery system was tailored to fit within a Stark exemption. CMS views these pod labs as abusive and will apply the (anti-markup) rule to those labs."
However, on March 31 a federal court in Washington, DC, placed a preliminary injunction against the CMS at the request of plaintiffs, which include Florida-based Atlantic Urological Associates, to delay implementation of the policy against the pod labs.
By Wayne Forrest
AuntMinnie.com staff writer
April 14, 2008
Related Reading
New CMS rules alter practices in independent imaging centers, April 8, 2008
CMS delays in-office self-referral decision with new MPFS rule, November 7, 2007
CMS publishes 2008 physician payment rule, November 4, 2007
New CMS rules could add to radiology's reimbursement woes, August 1, 2007
CMS releases 2008 HOPPS proposed rule, July 19, 2007
Copyright © 2008 AuntMinnie.com