Technology-enabled interventions could help reduce unnecessary recommendations for additional imaging (RAIs), according to findings published June 3 in Radiology.
Researchers led by Ramin Khorasani, MD, from Harvard Medical School in Boston, MA, found that when these interventions were implemented at a site, the rate of RAIs decreased by 44%. This can reduce the rates of clinically unnecessary RAIs and improve recommendation clarity and actionability, they highlighted.
“Such changes have the potential to improve patient safety, decrease health care costs, yield fewer diagnostic errors, and reduce low-value imaging follow-up,” Khorasani and colleagues wrote.
Ambiguous or unnecessary RAIs can result in the overuse of imaging, diagnostic errors, and increased costs. Furthermore, between one-quarter and two-thirds of RAIs may not be acted on by referring providers. Reasons include patient clinical factors and preferences that are unknown to the interpreting radiologist and a lack of systems to ensure timely performance of clinically necessary RAIs.
The Khorasani-led team investigated the cumulative impacts of multifaceted technology-enabled interventions on RAI rate, actionability, and resolution over an eight-year period between 2015 and 2022.
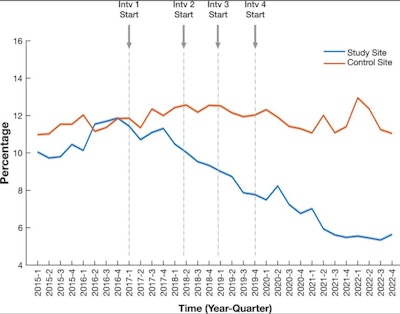 The graph shows the rate of recommendations for additional imaging in radiology reports over time at the study and control sites during the eight-year study period. Intv = interventionRSNA
The graph shows the rate of recommendations for additional imaging in radiology reports over time at the study and control sites during the eight-year study period. Intv = interventionRSNA
The team analyzed radiology reports from two tertiary hospitals and introduced a series of quality improvement interventions to one site (study site). These interventions included the following: radiologist education, electronic communication tools for tracking RAIs, and performance reports. The team compared results from both the study site and control site, the latter of which received no interventions.
Final analysis included over 7.5 million total radiology reports from 1.3 million patients. The study included 3.6 million reports from 660,051 patients, while the control site had about 2.9 million reports from 690,115 patients.
Although the control site remained mostly unchanged throughout the study period, the study site experienced a significant reduction in its RAI rate.
Comparison between sites that were with, without interventions toward RAIs | ||
Measure | Control site | |
Year | 2015 | 2022 |
RAI rate | 10.9% | 11% |
| *Data comparing the control site and study site achieved statistical significance. | ||
RAI rates also declined with each successive intervention at the study site (p < 0.001). Regression coefficients decreased from −0.12 for the initial intervention to −0.81 for the final intervention, the team reported.
Recommendation actionability at the study site increased 7.6-fold, from 5.6% to 42.3% (p < 0.001). However, at the control site, this trend remained unchanged with a decrease from 15.0% to 13.8% (p = 0.73).
Finally, the researchers found that actionable RAIs were more often resolved at the study site than at the control site (84.7% vs. 59.6%; p < 0.001).
The study authors highlighted that their results point to the impact of introducing such interventions on patient safety by reducing diagnostic errors and increasing follow-through on actionable RAIs.
“Furthermore, this initiative may help streamline imaging practices and contribute to more judicious use of imaging resources,” they wrote.
The team also highlighted that since the study, the interventions have been extended across the team’s entire healthcare system. It is also assessing whether generative AI tools can be used in the program’s workflows.
This approach could help medical centers and practices that may be challenged by limited resources, according to an accompanying editorial written by Eric Russell, MD, from Northwestern University in Chicago, IL.
“Their institution is to be commended for their success, and hopefully others will invest the resources needed to follow their lead,” Russell wrote. “Questions remain, including how to sustain continued institutional commitment to preserve the gains made during the study period, particularly regarding continuous ongoing education and monitoring of newly onboarded radiologists.”
He suggested that future studies could include financial analysis to track any potential savings that may offset implementation costs, and that AI-driven strategies may further help.
The full study can be found here.




















