Using deuterium metabolic imaging (DMI) data for metabolic modeling could provide insight into epilepsy and glioblastoma, suggest findings presented May 12 at the International Society for Magnetic Resonance in Medicine (ISMRM) 2025 meeting in Honolulu, HI.
In her presentation, Evita Wiegers, PhD, from University Medical Center Utrecht in the Netherlands, spoke on behalf of her team, highlighting how metabolic modeling with DMI can estimate the tricarboxylic acid cycle rate in both healthy and diseased brain tissue.
“We demonstrated the potential of metabolic modeling with DMI data in healthy, epilepsy, and brain tumor patients,” Wiegers said.
Epilepsy and glioblastoma are known to affect brain glucose metabolism. F-18 FDG-PET is used to detect hypometabolism in patients with epilepsy, and carbon-13 (C-13) MR spectroscopy in metabolic modeling can estimate neurotransmitter cycling.
However, the researchers aimed to introduce a less invasive and more feasible method for metabolic modeling. They used DMI in their model, citing the modality’s whole-brain coverage and being less costly than C-13 MR spectroscopy.
With this in mind, the team studied brain glucose metabolism across tumor tissue, epileptogenic tissue, and healthy brain tissue, focusing on the tricarboxylic acid cycle rate.
The prospective study included five healthy volunteers, five MRI-negative PET-positive epilepsy patients, and five newly diagnosed glioblastoma isocitrate dehydrogenase (GBM IDH) wildtype patients. The team also employed a 7-tesla MR scanner (Philips), an in-house developed head coil consisting of eight hydrogen-2 (H-2) receive loop coils and eight hydrogen-1 transmit/receive dipole antennas, and a custom-built H-2 transmit bore coil.
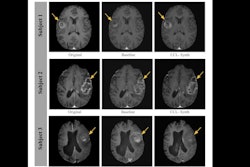
 A research team out of University Medical Center Utrecht in the Netherlands described their DMI metabolic modeling approach at ISMRM 2025. It found differences in brain tissue between healthy, epilepsy, and brain tumor patients.ISMRM
A research team out of University Medical Center Utrecht in the Netherlands described their DMI metabolic modeling approach at ISMRM 2025. It found differences in brain tissue between healthy, epilepsy, and brain tumor patients.ISMRM
The team reported that plasma deuterium glucose levels were similar across all patient and volunteer groups. However, deuterium glutamate levels in glioblastoma were lower than those of the other two groups.
Analysis of variance and post-hoc analysis showed higher tricarboxylic acid cycle rates in the healthy volunteers compared with glioblastoma tissue (p = 0.01).
Finally, the team reported no significant difference between epileptogenic tissue versus normal appearing brain tissue (p = 0.69) and glioblastoma versus normal appearing brain tissue (p = 0.11).
Wiegers said the results highlight the potential of DMI for metabolic modeling in measuring disease extent in patients with epilepsy and glioblastoma. However, she cautioned that the model results should be interpreted carefully since it relies on assumptions and simplifies brain metabolism. She added that the regions of interest were drawn with “limited precision.”
Check out AuntMinnie’s full coverage of ISMRM 2025 here.