Musculoskeletal Tumors:
Histologic grade reflects biologic behavior of bone and soft-tissue sarcomas is incorporated into their staging classification [14]. FDG uptake is typically related to degree of tumor dedifferentiation and FDG-PET can be used to evaluate musculoskeletal tumors. FDG exams can detect distant metastases, evaluate for recurrence, and monitor response to therapy. PET/CT has been shown to be more accurate than PET alone for the staging of bone and soft tissue scaromas [14]. Combined PET/CT imaging resulted in correct N-staging in 96% and correct M-staging in 91% of patients, compared to 91% and 79% respectively for conventional imaging alone [14]. Combine PET/CT and conventional imaging results in overall correct staging in up to 87% of patients [14]. Combined PET/CT and conventional imaging can help to alter treatment in up to 14% of patients (compared to conventional imaging alone) and preclude surgical resection in up to 13% of patients [14].
Primary tumor evaluation:
SUV values can be helpful in distinguishing benign from malignant lesions. However, increased FDG uptake in a skeletal lesion is not pathognomonic for a malignant neoplasms [5,8]. Increased tracer accumulation has been described with benign bone lesions (including non-ossifying fibroma, fibrous dysplasia, giant cell tumors, eosinophilic granuloma, and aneurysmal bone cyst) and at sites of inflammation or infection.
PET FDG false negative examinations have been reported in association with malignant lesions- particularly chondrosarcomas and plasmacytomas, but also low grade osteosarcomas and Ewing's sarcoma [1,5]. False-negative exams can also occur for low grade soft-tissue sarcomas which tend to have low FDG uptake [3].
In a meta-analysis of FDG PET data in the evaluation of soft-tissue lesions the sensitivity and specificity for malignant versus benign lesions was 87% and 79%, respectively using an SUV value of 2.0 (visual quantification was 92% and 73% respectively) [8]. FDG images are generally positive in intermediate and high grade tumors (CI: 97-100%), but uptake is less consistent in low grade lesions (74%, CI: 59-86%) [8].
Response to therapy:
Perhaps, one of the more important applications of FDG PET is in evaluation of response to therapy. Chemotherapy and radiation can be used pre-operatively to decrease tumor size in order to facilitate the limited resection needed for limb-salvage surgery [2]. The correlation between histopathologic tumor necrosis after preoperative chemotherapy with clinical prognosis is well established [2].
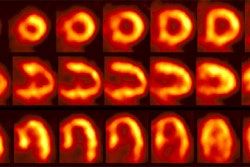
Functional imaging with FDG PET allows detection of biochemical changes within the lesion prior to visible morphological changes. A decrease in the tumor to non-tumor uptake ration of greater than 30% after chemotherapy has been shown to correlate well with extensive histologic tumor necrosis [2]. For patients that fail to demonstrate a response to treatment, early therapy modification can be performed. This is important as post-operative modifications in therapy regimens for non-responders have not been shown to improve patient outcome [2].
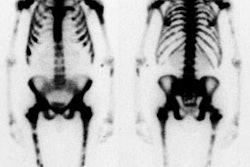
FDG PET imaging is superior to bone scintigraphy for evaluation of tumor response to therapy as bone healing (sclerosis) will result in increased Tc-99m-accumulation ("flare" phenomenon) [2].
Following completion of therapy, MR imaging can often be equivocal in differentiating post-therapy changes from tumor recurrence. FDG PET imaging has shown promise in the ability to identify recurrent tumor [7]. When positive in these cases, results of the PET exam can be used to guide biopsy of the most metabolically active regions [7].
18F-labeled NaF (sodium fluoride) may hold promise for the identification of bone metastases with improved lesion detection compared to bone scan [4].
Specific tumors:
Osteosarcoma:
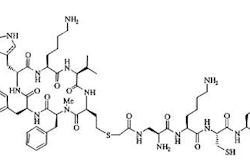
Combined Fluorine-18 (blood flow and osteoblastic response) and FDG (metabolism) imaging can be combined to evaluate primary bone neoplasms. In patients with osteosarcoma, increased uptake of both agents is identified in a distribution corresponding to the bone and soft tissue components of the tumor respectively.
In general, there is good correlation between the amount of FDG uptake and the histologic grade of the lesion. A high tumor FDG uptake has also been shown to correlate with a poor prognosis [6]. Following successful neoadjuvant chemotherapy tumor FDG uptake will decrease [6]. F-18 uptake will still be seen in areas corresponding to sclerosis, but regional accumulation of FDG in these areas will be normal [4].
Giant cell tumors:
Giant cell tumors are usually classified as benign lesions, however, they frequently demonstrate local recurrence (up to 50%) and metastatses may occur [9]. Giant cell tumors have generally enhanced FDG uptake- mean SUV 4.8 [9].
Childhood sarcomas:
FDG PET imaging can detect unsuspected sites of metastatic disease and can be used to monitor response to therapy [10].
Benign fibrous lesions:
Benign fibro-osseous lesions such as non-ossifying fibromas or fibroxanthomas (which are referred to as a fibrous cortical defect when smaller than 3 cm in size [13]), fibrous cortical defects, and cortical desmoids can all demonstrate FDG uptake [11,12,13]. Non-ossifying fibromas and fibrous cortical defects occur in 20-40% of children and are most commonly located in the metaphysis or diametaphyseal junction of the distal femur or proximal tibia [11]. The lesions appear as a radiolucent defect with a thin sclerotic border that is usually scalloped and slightly expansile [13]. The lesions generally undergo progressive ossification/spontaneous regression over time and are often no longer apparent after the second decade of life [11,13]. During their involutional phase, there is increased osteoblastic activity as the lesion is replaced by new bone [11]. Non-ossifying fibromas tend to take longer to regress than do fibrous cortical defects [11]. Cortical desmoids are located on the posteromedial surface of the distal femur at the site of attachment of the extensor tendinous fibers of the adductor magnus muscle- they are the result of repetitive traction microavulsions with a subsequent fibroblastic response [11]. Cortical desmoids are found in about 11% of boys and 4% of girls [11].
All of the above fibroosseous lesions can appear metabolically active on FDG PET imaging [11]. Uptake on the PET scan also does NOT necessarily correlate with increased uptake on bone scan (i.e.: the lesion may not appear active on bone scan) [11].
REFERENCES:
(1) J Nucl Med 2000; Schulte M, et al. Grading of tumors and tumorlike lesions of bone: Evaluation by FDG PET. 41: 1695-1701
(2) Clin Nucl Med 2000; Franzius C, et al. Evaluation of chemotherapy response in primary bone tumors with F-18 FDG positron emission tomography compared with histologically assessed tumor necrosis. 25: 874-881
(3) J Nucl Med 2001; Dimitrakopoulou-Strauss A, et al. Dynamic PET 18F-FDG studies in patients with primary and recurrent soft-tissue sarcomas: Impact on diagnosis and correlation with grading. 42: 713-720
(4) J Nucl Med 2001; Schirrmeister H, et al. Prospective evaluation of the clinical value of planar bone scans, SPECT, and 18F-labeled NaF PET in newly diagnosed lung cancer. 42: 1800-1804
(5) J Nucl Med 2002; Dimitrakopoulou-Strauss A, et al. The role of quantitative 18F-FDG PET studies for the differentiation of malignant and benign bone lesions. 178: 510-518
(6) J Nucl Med 2002; Franzius C, et al. Prognostic significance of 18F-FDG and 99mTc-methylene diphosphonate uptake in primary osteosarcoma. 43: 1012-1017
(7) AJR 2002; Bredella MA, et al. Value of FDG positron emission tomography in conjunction with MR imaging for evaluating therapy response in patients with musculoskeletal sarcomas. 179: 1145-1150
(8) J Nucl Med 2003; Ioannidis JPA, Lau J. 18F-FDG PET for the diagnosis and grading of soft-tissue sarcoma: a meta-analysis. 44: 717-724
(9) J Nucl Med 2004; Strauss LG, et al. 18F-FDG kinetics and gene expression in giant cell tumors. 45: 1528-1535
(10) AJR 2005; McCarville MB, et al. PET/CT in the evaluation of childhood sarcomas. 184: 1293-1304
(11) AJR 2006; Goodin GS, et al. PET/CT characterization of fibroosseous defects in children: 18F-FDG uptake can mimic metastatic disease. 187: 1124-1128
(12) AJR 2006; Iagaru A, Henderson R. PET/CT followup in nonossifying fibroma. 187: 830-832
(13) Radiology 2007; Hetts SW, et al. Case 110: Nonossifying fibroma. 243: 288-292
(14) Radiology 2007; Tateishi U, et al. Bone and soft-tissue sarcoma: preoperative staging with fluorine 18 fluorodeoxyglucose PET/CT and conventional imaging. 245: 839-847