PET CNS Imaging:
Seizure Disorders:
(For more extensive discussion, see Tc-HMPAO seizure imaging in CNS section)
Epilepsy is one of the most prevalent neurological
disorders affecting 0.5-1% of the general population [34]. Seizures can be classified as either partial (focal) or generalized.
Partial seizures originate in a given area of the brain and can be divided into
simple (with no impairment of consciousness) and complex (with impairment of
consciousness). Most partial complex seizures originate in the temporal lobe.
The majority of patients can be treated effectively with antiepileptic drugs,
but up to 20% of patients with seizure disorders (and over 40% of patients with
complex partial seizures) may be inadequately controlled [34]. Patients unresponsive to anti-convulsant
therapy may be candidates for surgical treatment- particularly those with
temporal lobe epilepsy. Surgery can decrease (in up to 92% of patients) or
eliminate (up to 68% of patients) seizure episodes, however, accurate
localization of the seizure focus is key for a successful post surgical outcome
[34]. Unfortunately scalp EEG often fails to
accurately localize the seizure focus. Depth EEG is much more accurate, but it
is also extremely invasive (requiring a craniotomy) and suffers from regional
under sampling.
PET is very sensitive in the early detection of the functional disturbance associated with microscopic neuronal disorganization which results in epilepsy. During the interictal phase, PET imaging with FDG will demonstrate a zone of decreased glucose utilization and decreased cerebral blood flow (CBF) at the site of a seizure focus in 60 to 70% of patients with normal MRI exams [5]. In patients with intractable temporal lobe epilepsy, interictal PET shows the hypometabolism near the seizure focus in 86% of patients [34]. The distribution of the PET abnormality correlates very well with the extent of the epileptogenic zone as determined by intraoperative EEG, but correlates poorly with the extent of morphological abnormalities in the resected specimen- the area of hypometabolism is often much larger than the actual area of structural abnormality. Among patients undergoing temporal lobectomy, a quantitative asymmetry index of greater than 15% for the lateral temporal lobe indicates the patient will likely have a good surgical outcome [6].
Other PET agents have also been studied for the evaluation of seizures. Benzodiazepine receptor imaging will demonstrate decreased activity within the involved medial temporal cortex [29]. Opiate receptor imaging will demonstrate increased tracer uptake in regions of decreased FDG accumulation corresponding to the seizure focus [29].
Inter-ictal FDG PET exam: The patient in the case below suffered from intractable drop seizures since the age of 18 months. An MRI was normal. Ictal scalp EEG demonstrated epileptiform activity emanating from the right parietal region. The FDG PET exam revealed a region of hypometabolism (red arrow) in the right parietal lobe. The PET exam guided subdural grid placement with very good correlation. The patient underwent surgical treatment and became seizure free. The exam was performed on an ECAT EXACT HR+ (manufactured by CTI). Case courtesy of Harry Chugani, M.D., Childrens Hospital of Michigan, and CTI PET Systems, Inc. |
In patients with Sturge-Weber syndrome, FDG typically shows widespread unilateral hypometabolism ipsilateral to the facial nevus [11]. In infants less than 1 year of age, however, the interictal scan often shows a paradoxical increased cortical metabolism ipsilateral to the facial nevus [11].
Cerebrovascular Disorders
Physiology, radiopharmaceuticals, and the PET exam:
Cerebral blood volume, cerebral
blood flow, the cerebral metabolic
rate of oxygen, and cerebral metabolic rate of glucose all reflect various
aspects of cerebral homeostasis. Derangements in cerebral perfusion produce
alterations in this homeostasis that can be images with PET agents.
Cerebral blood volume:
With PET imaging, the regional distribution of cerebral blood volume (CBV) is
imaged following the inhalation of C-11 (T1/2= 20.3 min.) or O-15 carbon
monoxide (CO). Radiolabeled CO binds with high affinity to hemoglobin within red
blood cells (forming carboxyhemaglobin) permitting absolute measurements of CBV.
Images of CBV show the greatest concentration of activity in the dural venous
and carotid sinuses. Although blood accounts for only 5% of the volume of the
gray matter structures, the gray matter has a larger CBV than the white matter. The
normal whole brain CBV value is 4.2 ml/100gm.
Vasodilatation is an early
response to cerebral arterial occlusion and can be used to identify areas of
decreased perfusion pressure. The ratio of CBV/CBF (cerebral blood flow)
increases as cerebral perfusion pressure falls.
Cerebral blood flow:
In the healthy brain, cerebral blood flow is normally tightly coupled with local
metabolic needs [28]. Cerebral blood flow (CBF) can be measured by using O-15 water intravenously (for
scanners with high count rate capabilities), O-15 carbon dioxide inhaled (for
scanners with limited count rate capabilities), or C-11 butanol. O-15 labeled
carbon dioxide is converted to radiolabeled water by the action of carbonic
anhydrase. The whole brain mean CBF is
between 40-50 ml/100 gm/min. The gray matter CBF is 2.5 to 3 times
greater than that of the white matter (56 versus 20 ml/100gm/min.). Electrical
activity in the brain diminishes at CBF values below 20 ml/100gm/min. and cell
death occurs when the CBF falls below 10 ml/100gm/min.
Cerebral metabolic rate of
oxygen: The cerebral metabolic rate of
oxygen (CMRO2) is measured using O-15 oxygen. A
normal mean regional CMRO2
is approximately 3.0 ml O2/100gm/min.
A minimum value of at least 1.3-1.5 ml O2/100gm/min. is required for
tissue viability. CMRO2 is calculated from measurements of CBF, CBV,
and the oxygen extraction fraction (OEF).
The OEF represents the fraction
of oxygen extracted from the blood by the brain in a single capillary transit
and is approximately equal to 0.4. OEF increases as blood flow decreases. OEF is
calculated by using O-15 labeled O2 (O15O). Labeled O2 is
extracted by the brain and immediately metabolized to H2 15O.
OEF=
CMRO2 / CBF [arterial O2
concentration]
Cerebral metabolic rate for
glucose: Either F-18 fluorodeoxyglucose or C-11 deoxyglucose can be used to
determine cerebral metabolic rate for glucose (CMRglu). Unfortunately, C-11
deoxyglucose is a less than optimal agent, because it is metabolized and the
C-11 rapidly leaves the brain in the form of labeled CO2. FDG crosses
the blood brain barrier by a carrier mediated transport mechanism similar to
those operating for glucose. The agent is phosphorylated into hexokinase, but
not further metabolized and it remains inside the neural cell.
Images are performed
approximately 40-60 minutes after tracer injection at which time most blood-pool
activity has cleared.
There is generally homogeneous regional
utilization of glucose within the gray matter
structures of normal resting individuals (although a decline in frontal
metabolism has been reported with age).
Cerebral Infarction
In a normal resting brain,
cerebral blood flow, glucose metabolism, and the cerebral metabolic rate for O2
are linked by a constant relationship and the OEF is relatively homogeneous
across the brain..
In the early phase of CVA or
reduced cerebral perfusion pressure, blood flow is maintained through
autoregulated arteriolar vasodilatation leading to an increase in regional
cerebral blood volume (CBV) [10,28]. When the vascular response is
maximal and no further dilatation is possible, rCBF will begin to decrease,
however, regional oxygen extraction fraction (rOEF) will begin to increase in an
effort to maintain a stable CMRO2 [10]. With mild to moderate
decreases in CBF, neuronal function can be maintained without compromise so long
as OEF increases to maintain CMRO2. In severe decreased blood flow (as CBF falls
below 15-18 ml/100gm/min.), oxygen extraction rises to maximal levels. Further
decreases in perfusion will then lead to the onset of ischemia and a decrease in CMRO2. The
presence of increased OEF has been shown to be a powerful and independent
predictor of subsequent stroke in patients with atherosclerotic cerebral
vascular disease [7].
Regions with CBF below 11
ml/100gm/min. almost always proceed to tissue necrosis. Focal reductions in CBF
and CMRO2 mimicking acute infarction can be seen in patients with
other disorders such as cerebral hemorrhage, multiple sclerosis, or infiltrating
tumor. In general, CMRglu measured with FDG tends to be lower in a site of
hemorrhage compared to acute ischemic infarction, although there is considerable
overlap.
In most cases of acute ischemic stroke, the CMRglu is reduced in the affected tissue; however, CMRglu may be increased above normal gray matter in some sections of the infarction in up to 10% of cases probably secondary to increased anaerobic glycolysis. In general, CMRglu is reduced less than CMRO2. During acute ischemia the CMRO2 appears to be the most important determinant of tissue viability. During the early portion of the post-infarction period, depending on the site and severity of obstruction, ischemic cerebral tissue may be salvageable. Tissue pH is reduced under conditions of acute ischemia, but is typically alkalotic by 5 days following the infarction.
By one week post infarction there is a reversal of the previous pattern noted- with persistent vasodilatation there is increased rCBF associated with decreased or unchanged glucose utilization due to decreased demand for oxygen metabolism in infarcted brain tissue [10,28. This uncoupling of flow and metabolism in which the CBF exceeds metabolic demands represents luxury perfusion. By one month post-infarct, a matched decrease in rCBF, rCMRO2, and glucose metabolism is seen indicating irreversibly infarcted tissue. Arteriovenous malformations (AVMs) also create a situation in which local blood flow greatly exceeds local oxygen utilization and cannot be distinguished from a subacute infarction with luxury perfusion by PET imaging.
| Condition | CMRO2 | CBV | OEF | CBF | CMRglu |
| Decreased flow reserve | Normal | Increased | Increased | Maximum possible | Normal |
| Acute ischemia | Decreased | Increased | Increased | Decreased | Generally reduced |
| Late infarct | Decreased | Variable | Normal | Decreased | Decreased |
PET imaging has also demonstrated widespread metabolic changes in structures remote form the site of infarction [10]. Crossed cerebellar diaschisis refers to a decrease in cerebellar blood flow and oxygen metabolism contralateral to the site of cerebral infarction during the first 2 months post event [10]. Interruption of the cerebro-ponto-cerebellar pathway is the proposed mechanism for this finding. Other remote function effects include decreased metabolism in the ipsilateral thalamus and caudate [10]. A decline in metabolic activity in the primary visual cortex ipsilateral to an infarct which involves the anterior visual pathways reflects a clinical homonymous hemianopsia.
Multi-infarct Dementia
MID is characterized by multifocal, asymmetric matched reductions of rCBF and rCMRglu corresponding to the locations of cortical and subcortical infarcts [8].
Arteriovenous Malformations
These lesions classically demonstrate increased regional cerebral blood volume ipsilateral to the malformation, associated with significantly decreased glucose metabolism.
Neuropsychiatric Disorders:
Dementia:
PET imaging has been used for the assessment of dementia. When performing quantitative measurements on PET exams performed on elderly patients for dementia, it is important to remember to correct for age-related volume loss. Partial-volume averaging due to expanded sulci can result in PET measurements that underestimate true values [1]. When such corrections are made, it can be demonstrated that there is no decline in cerebral blood flow in healthy elderly individuals (except for the oribitofrontal cortex) [1,2]. A decline in dopamine activity with age, however, has been documented [2].
Clinical:
Alzheimer disease (AD) is a progressive neurodegenerative disorder associated with gradual deterioration in cognition, function, and behavior [16]. Decreasing mortality with an ever greater elderly population has led to a rising prevalence of senile dementia [4]. The prevalence of AD is below 1% in people aged 60-64y, but shows an almost exponential increase with age [35]. It is estimated that 8% of people over the age of 65 years suffer from Alzheimer's disease and the prevalence climbs with increasing age (about 30% in patients over the age of 85 years) [15,16]. The female to male prevalence of AD is 70%- likely related to the longer life expectancy of women [35]. Alzheimer's disease (AD) affects over 4 million people in the United States and the condition is tremendously costly to patients, their families, and society [4]. AD progresses incidiously with initial sparing of sensory and motor function [15,16]. Unfortunately, the condition frequently goes unrecognized or is not properly clinically diagnosed until it's more advanced stages [15,16]. Recent studies have identified certain genetic risk factors for Alzheimer's disease. Apolipoprotein (APOE), a gene on chromosome 19, has been reported to have an association with AD. The presence of APOE-4 allele increases the risk for AD, while the APOE-2 allele appears to have a protective effect. Patients with the APOE-4 allele may prove to benefit from early PET imaging in order to identify changes suggestive of AD prior to the onset of clinical symptoms. A rare familial form of AD also exists with autosomal dominant inheritance and nearly 100% penetrance [32].
A need for accurate, early diagnosis is very important as medications (cholinesterase inhibitors such as Donepezil hydrocholride) are now available that have been shown to improve or delay the memory and other cognitive loss that occurs in mild to moderate disease [15,16,20,35]. A delay in the implementation of therapy may also have long term consequences [20]. Patients with AD in whom the start of cholinesterase inhibitor therapy is delayed demonstrate fewer benefits than do patients starting therapy early in the course of AD [35].
Pathology:
Pathologically AD is characterized by a reduction in the number of large cortical neurons in the temporal and frontal cortex and by the appearance of senile or amyloid plaques (extracellular deposits of beta-amyloid protein) and neurofibrillary tangles (intyracellular aggregates of tau proteins that interfere with the assembly and stability of the neuroskeleton) [16,38]. Cerebral metabolic rate for glucose primarily reflects neuronal and synaptic activity, and at autopsy patients with Alzheimer's are found to have an average decrease of 50% in the density of the granular neurophil in the parietal and temporal cortices [8]. The greatest density of neuritic plaques and neurofibrillary tangles are also found in these locations [8].
PET imaging in Alzheimer's disease:
FDG PET can improve diagnostic accuracy in the evaluation of patients with cognitive decline (mild cognitive impairment or MCI). Patients with mild cognitive impairment are at a 10 times higher risk for developing dementia compared to the general population [35]. PET FDG imaging is currently used primarily as an adjunct to the clinical determination of AD and is especially useful in differentiating AD from other dementias (including vascular dementia). [16,17]. FDG PET imaging has demonstrated promise in providing a diagnosis of AD 2 to 3 years before full dementia-related symptoms manifest [16]. This observation of a reduction in metabolism in presymptomatic patients indicates that the pathophysiologic process begins before the condition is recognized clinically [35]. By confirming the diagnosis of AD, PET imaging allows for the early institution of appropriate therapy. Also- patients with negative PET scans, can be spared the expense of unnecessary treatment. Presently, the available literature would also support the use of PET imaging for at least 2 groups of patients- those with mild or moderate cognitive impairment who meet the standard criteria for dementia (the cause of which has not been identified by an appropriate medical workup); and those patients with mild or moderate cognitive impairment who exhibit progressive cognitive dysfunction that has not reversed after a thorough medical workup [20].
Findings in AD: AD classically produces a pattern of bilateral parietotemporal hypometabolism [3] (which can be asymmetric early in the course of the disease [16,20]) even before substantial abnormalities appear on clinical or neuropsychiatric tests [8]. There is relative sparing of the basal ganglia, thalamus, cerebellum, and cortex mediating primary motor and sensory functions [20]. The combination of reduced metabolic activity in a suspicious distribution and genetic risk factors provides a means for the detection of pre-clinical disease [18].
PET FDG imaging has been shown to have a sensitivity of 92-96%, specificity of 63-89%, and an accuracy of 82-90% for the confirmation of Alzheimer's in patients that are difficult to characterize on clinical evaluation [3,4,25]. In another study of 138 patients with a pathologically confirmed diagnosis, PET correctly identified the presence or absence of AD in 88%, with a sensitivity of 94% (89-99%; 95% CI), and a specificity of 73% (60-87%, 95% CI) [17]. The patients in this study were generally felt to have mild cognitive impairment at the time of their initial PET exam [17]. In another prospective study of patients with mild cognitive impairment (MCI) [25], PET correctly identified patients that would progress to Alzheimer's with a sensitivity of 92% and a specificity of 89%. However, the high conversion rate from MCI to AD in this study (40%) may have contributed to the very high sensitivity [25]. This study also used an automated image analysis program (NEUROSTAT) to aid in image interpretation [25]. Programs such as NEUROSTAT provide advantages in objectivity, reproducibility, and speed of image anaylsis as a result of automatic anatomic standardization and statistical processing [26]. PET imaging can also improve the accuracy in identifying early Alzheimer's without adding to the overall costs of diagnosis and treatment [15]. In patients presenting with cognitive symptoms, a negative PET indicates a lower likelihood for a progressive dementia with a specificity of about 76% [17]. In a meta-analysis of PET data in Alzheimer's disease, the summary sensitivity was 86% (95% CI: 76%-93%) and the summary specificity was 86% (95% CI: 72%-93%) [19].
When compared to SPECT imaging, reductions in tracer activity are significantly more pronounced for PET imaging [14]. The magnitude of the deficits on PET also correlates with the degree of cognitive impairment [16] and the correlation between dementia severity and the number of abnormal voxels is closer for PET than for SPECT [14]. Metabolic activity in the primary sensory-motor cortex, basal ganglia, thalamus, and cerebellum are typically normal in patients with Azlheimer's disease [16]. Overall, for the detection of AD, PET has an increased accuracy of 15-20% compared to SPECT imaging [20].
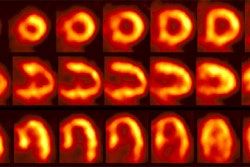
Alzheimer's disease on FDG PET: The case below is from an 86 year old male being imaged to exclude Alzheimer's disease. The FDG PET exam demonstrated bilateral temporoparietal hypometabolism. This finding is very sensitive for the diagnosis of Alheimer's disease. The exam was performed on an ECAT EXACT HR+ PET scanner (manufactured by CTI) after administration of 108 MBq FDG. The exam was acquired using a 3D dynamic emission and 15 minute transmission protocol. Case courtesy of Institut fur Medizin Forschungszentrum Julich, Germany and CTI PET Systems, Inc. |
The pattern of biparietotemporal hypometabolism is not absolutely pathognomonic for Alzheimer's and can also be seen in patients with Parkinson's disease with dementia [20], bilateral parietal subdurals [8], dementia with Lewy bodies (but will also involve the visual cortex) [16], Creutzfeldt-Jacob disease [3], or biparietotemporal infarctions [8].
The global CMRglu has also be evaluated in patients with AD and is reduced in up to 35% of Alzheimer's patients. However, this may also be seen in patients with depression, Parkinson's, following convulsion, trauma, cerebral irradiation, ECT therapy, and with drug induced impairment of consciousness. CMRglu also decreases normally in the elderly, despite maintenance of CBF, and CMRO2.
Abnormalities within the cholinergic system have been consistently identified in patients with Alzheimer's. There is a 40 to 90% decrease in the enzyme choline acetyltransferase and consequently in acetylcholine levels within the cerebral cortex. In contrast, the dopaminergic system is not abnormal in Alzheimer's patients (as it is in patients with Parkinsons).
New radiotracers may hold promise for imaging patients with AD [16]. The agent [18F] FDDNP targets amyloid senile plaques and neurofibrillary tangles and will show increased temporal-parietal accumulation of the tracer in AD [16]. The greater degree of tracer accumulation correlates with memory performance scores and decreased glucose metabolism on FDG PET imaging [18].
Frontotemporal dementia (Pick's Disease):
Frontotemporal dementia (FTD) is another cortical dementia which is less common than Alzheimers disease [8,21]. FTD is a heterogenenous clinicopathologic syndrome caused by progressive degeneration of the frontal and anterior temporal lobes [8,21,35]. FTD usually presents with changes in personality, language, and behavior, with memory dysfunction not occurring until later [8,27]. At autopsy, there is frontal and temporal atrophy with neuronal loss, gliosis, inflated neurons, and Pick bodies [8]. Hypometabolism in the frontal and anterior temporal lobes is the characteristic finding [21]. Other areas that may be involved include the cingulate gyrus, uncus, insula, basal ganglia, and thalamic regions [35]. The hypometabolism is frequently asymmetric and worse on the left [21].
Parkinson's is a neurodegenerative disorder resulting from the progressive death of dopaminergic neurons in the nigrostriatal pathway (pars compacta of the substantia nigra and locus ceruleus, and presynaptic dopaminergic nerve terminals in the caudate nucleus and putamen) [8,12]. Symptoms consist of rigidity, bradykinesia, difficulty in initiating and stopping movement, and a resting tremor [8].
Motor disturbances begin only after a loss of approximately 70-80% of striatal dopamine- thus, there is a long latent period which precedes the development of clinical symptoms [12]. Approximately 10% of patients with Parkinson's develop a dementia [8]. The dementia associated with Parkinson's seems to produce a uniform cerebral hypometabloism, however, biparietal hypometabolism identical to Alzheimer's can also seen in these patients (this finding is typically not found in Parkinson's patients without dementia) [8,27].
L-dihydroxyphenylalanine (L-DOPA) is the immediate precursor of dopamine [36]. L-DOPA is carried into the brain by the large neutral amino acid transport system, converted into dopamine by the action of L-aromatic amino acid decarboxylse, and then stored in intraneuronal vesicles [36]. The loss of dopaminergic nerve terminals in the basal ganglia can be detected by PET imaging with 6-[18F] fluoro-DOPA (an analog of L-DOPA]) to study the presynaptic component of the nigrostriatal dopamine system and dopamine metabolism [36]. The agent crosses the blood brain barrier where it is converted into 6-[18F]-fluoro-dopamine by the action of DOPA decarboxylase and stored in the presynaptic vesicles [23,38]. Unfortunately, 6-FD is also largely metabolized peripherally by DOPA decarboxylase (DDC) to 3-O-6 -[18F]-fluorodopamine which also crosses the BBB [23]. This factor, as well as other peripheral metabolites which may cross the BBB, complicate the quantification of brain uptake of 6-FD. Pre-treatment with inhibitors of DDC, such as Carbidopa, when injected before administration of the 6-FD improve brain uptake of the tracer considerably [22]. One other problem with [18F] fluoro-DOPA imaging is that the decardoxylating enzyme can be upregulated as a compensatory phenomenon , and the uptake of 18F-DOPA may be normal in patients with early disease [36,38].
The cerebral radioactivity measured after the administration of 6-FD is a function of uptake of the isotope into the brain and its subsequent metabolism to dopamine. In Parkinson's disease, the decrease in 6-FD accumulation is much more severe in the putamen than in the caudate nucleus [24]. Parkinson's patients with early disease and a continued response to L-dopa therapy retain 6-FD in the striatum better than patients with long-standing disease and a fluctuating response to therapy [30]. 6-FD imaging can also be used to monitor response to therapy and disease progression [30].
F-18 labeled derivatives of m-tyrosine have also been used to study Parkinson's disease. m-Tyrosine is a substrate for the enzyme aromatic amino acid decarboxylase which is responsible for the conversion of DOPA to dopamine. Marked reduction in activity within the basal ganglia (putamen and caudate) is seen in patients with Parkinson's disease with both 6-FD and m-tyrosine.
PET studies of alterations in D2 dopamine receptors have been conflicting. Patients that have been studied with C-11 N-methylspiperone while maintained on their usual dose of L-DOPA display essentially normal levels of dopamine receptors, despite the fact that F-18 fluoro-DOPA uptake is markedly reduced.
C-11 Nomifensine has been developed to study the dopamine reuptake system located on the presynaptic nerve terminals. This agent also demonstrates decreased uptake within the basal ganglia of Parkinson's patients.
Huntington's disease is a slowly progressive autosomal dominant neurodegenerative disorder characterized by choreiform (involuntary) movements, personality disorders, psychiatric symptoms, and dementia [8]. The age of onset is variable, but it occurs most frequently in the 3rd and 4th decades of life [8]. There is severe neuronal loss and atrophy of the caudate nuclei, and to a lesser extent the putamen and globus pallidus [8]. The caudate and putamen are deficient in the inhibitory neurotransmitter gamma aminobutyric acid (GABA) and glutamic acid decarboxylase.
FDG PET studies demonstrate decreased metabolic activity in the caudate, even when the CT is normal and years before the onset of motor symptoms [8,13]. Unfortunately, there is overlap of local caudate metabolic rates in patients at risk for Huntington's and normal control populations [13]. Global CMRglu tends to be normal in Huntington's patients, in contrast to Alzheimer's patients in which it is decreased.
Normal Pressure Hydrocephalus:
Clinically patients present with dementia, a gait disturbance, and urinary incontinence. ("Wet, wacky, and wobbly".) CT demonstrates moderate to severe enlargement of the frontal horns, obliteration of the sulci over the convexities, and periventricular hypodensities. The CSF pressure is normal. PET studies have demonstrated decreased metabolic activity compared to normal controls, but no regional deficit has been identified.
Dementia with Lewy Bodies:
Dementia with Lewy bodies (DLB) is a primary degenerative dementia characterized by the presence of Lewy bodies in cortical, subcortical, and brain stem structures [33]. It is the second most common degenerative dementia after Alheimer's disease- accounting for up to 20% of cases of dementia in older patients [33,35,37]. Patients present with the clinical triad of fluctuating cognitive impairment, recurrent detailed visual hallucinations, and Parkinson-like symptoms, or alterations in alertness and attention [16,35]. Two core features are necessary for a diagnosis of probable DLB, while the presence of one feature is consistent with possible DLB [37]. Based upon the clinical exam, the sensitivity for the diagnosis of probable DLB ranges from 22-83% (specificity from 79-100%) [37]. Cholinesterase inhibitors are currently the treatment of choice for DLB [16, 37]. However, neuroleptic medications can induce life threatening extrapyramidal reactions and should be avoided in DLB patients [37]. On FDG PET imaging there are bilateral temporal-parietal deficits similar to Alzheimers (AD), but the deficit also involves the occipital lobes (visual cortex) and cerebellum (areas typically spared in AD) [16]. Although reduced metabolic activity is seen in the occipital lobe, it is not affected histopathologically [33].
Progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome):
PSP begins in the 6th or 7th decade of life, and the duration of illness can range from 2 to 12 years [8]. Clinical signs include rigidity (which is more prominent axially than in the extremities), bradykinesia, supranuclear gaze palsies, pseudobulbar palsy, and frontal type dementia [8,30]. A clinical hallmark of the disorder is paralysis of vertical gaze, particularly in the downward direction [8].
Gross anatomic changes include atrophy of the brainstem (midbrain/pons), dentate nuclei of the cerebellum, and the cerebellar hemispheres to some degree [8]. There is an increase in aqueductal size, as well as in the size of the quadrigeminal, ambient, and crural cisterns [8]. Classically the condition produces a pattern of global reductions in cerebral oxygen and glucose metabolism that are most prominent frontal cortex [3,8].
PET imaging findings in Dementias [20]
| Dementia | PET findings |
| Alzheimer's | Decreased activity in the bilateral temporal and parietal cortices. During early stages, the defects often appear asymmetric. There is relative sparing of the basal ganglia, thalamus, cerebellum, and cortex mediating primary motor and sensory functions. |
| Vascular | Scattered defects in the cortical, subcortical, and cerebellar areas |
| Frontotemporal (Pick's) | Frontal cortex and anterior temporal and mesiotemporal decreased activity with sparing of the sensorimotor and visual cortices |
| Huntington's | Decreased activity in the caudate and lentiform nuclei (early) with gradual development of diffuse cortical involvement |
| Parkinson's with dementia | Deficits are similar to those of AD, but with more sparing of the mesiotemporal area and less sparing of the visual cortex |
| Dementia with Lewy bodies | Deficits are similar to AD, but with less sparing of the occipital cortex and possibly cerebellum |
Psychiatric disorders:
Schizophrenia
Schizophrenia represents a heterogeneous disorder [9]. The most frequently reported finding in patients with schizophrenia is decreased metabolic activity and decreased CBF in the frontal cortex- referred to as hypofrontality [9]. This finding is predominantly seen in patients with chronic schizophrenia that have a long history of neuroleptic treatment [9]. Studies have shown that chronic neuroleptic treatment increases whole brain metabolism, but this increase is less in the frontal lobes than other areas [9]. In contrast, younger patients may not demonstrate hypofrontality [9]. Hypofrontality is also more commonly identified in paranoid (45%), than non-paranoid schizophrenics (20%).
When challenged with an activation task such as the Wisconsin Card Sorting Test, most patients with schizophrenia demonstrate a failure of frontal lobe activation which is felt to be related to decreased dopamine function [9]. Because the frontal cortex is highly interconnected, an abnormality in this location may produce disturbances of activity in other cortical and subcortical structures. Unfortunately, frontal metabolic defects are not specific for schizophrenia and have also been identified in patients with affective disorders, chronic cocaine abuse, Parkinson's disease, supranuclear palsy, and advanced age [9].
Several tracers have also been used to measure dopamine receptors in schizophrenic patients and patients with Parkinson's disease: 18-F or 11-C N-methylspiroperidol (NMS), 11-C raclopride, F-18 spiperone, and Bromine-76 bromospirone. N-methylspiroperidol (NMS) is a potent antipsychotic drug that is pharmacologically similar to haloperidol. It binds to both dopamine D2 and serotonin S2 receptors (however, its binding affinity for Serotonin receptors is much lower than for the D2 receptors). D2 receptors exist on axons passing from the substantia nigra to the basal ganglia, while D1 receptors are found on axons passing from the cerebral cortex to these structures.
Following administration of NMS there is preferential accumulation of the tracer in the caudate nucleus and putamen which contain the highest densities of dopamine receptors (the corpus striatum is the site of greatest concentration of dopamine receptors in normal patients). Thalamic and cerebellar activity is low. C-11 raclopride is more sensitive to changes in dopamine concentration as it binds D2 receptors more selectively and has negligible binding to serotonin receptors. The agent can be used to monitor relative changes in synaptic dopamine concentration.
An increased number of D2 receptors in the caudate and putamen can be found in patients with untreated schizophrenia, however, patients with decreased dopamine D2 receptor concentrations have also been described. Because neuroleptics bind to dopamine receptors, the amount of available dopamine receptors demonstrated on PET imaging will reflect the amount of bound ligand (ie: NMS activity will decrease as greater amounts of the neuroleptic agent is bound). Patients receiving adequate treatment with neuroleptic drugs have approximately 90% of their dopamine receptors occupied (implying a near total blockage of dopaminergic neurotransmission). It was hoped that PET imaging could be used to identify patients that might not respond to neuroleptic therapy. Unfortunately studies have not been able to demonstrate a difference in receptor blockade between responders and non-responders [9].
The lack of consistent PET findings in patients with schizophrenia would suggest that schizophrenia is a heterogeneous disorder with subgroups of patients with different cerebral abnormalities.
Substance Abuse:
11-C labeled cocaine shows a heterogeneous distribution within the brain, with maximal uptake in the basal ganglia. Studies have also demonstrated that cocaine produces decreased metabolism in the cortical and subcortical structures [9], as well as widespread abnormalities in cerebral blood flow [9]. These flow abnormalities are probably the result of cocaine induced vasoconstriction, which can lead to tissue ischemia and infarction if severe [9]. The perfusion abnormalities are mostly localized to the frontal cortex, and cerebellar flow is generally unimpaired.
The region most commonly reported to be abnormal in metabolic studies of alcoholics is the frontal cortex [9]. Other studies during alcohol intoxication have demonstrated more heterogeneous decreases in metabolism, with the areas greatest affected being the occipital cortex, the cerebellum, and the prefrontal cortex- these areas also contain the highest concentration of benzodiazepine receptors in the brain [9]. Other areas which have relatively low concentrations of these receptors, such as the basal ganglia and corpus callosum, demonstrate only minimal metabolic changes following alcohol consumption.
C-11 Carfentanyl has a high affinity for mu opiate receptors which mediate analgesia and respiratory depression. The highest concentration of opiate receptors exist in the thalamus (highest concentration of mu receptors), striatum (caudate nucleus), and amygdala. There are very low concentrations of opiate receptors in the motor-sensory and occipital cortex. The distribution of the tracer can be changed by the prior administration of naloxone (an opiate antagonist) which results in markedly decreased uptake of the agent. C-11 carfentanyl studies of patients with partial complex seizures have demonstrated increased opiate receptor binding in the temporal lobe containing the epileptic focus (corresponding to the area of decreased glucose utilization identified on FDG imaging).
REFERENCES:
(1) J Nucl Med 2001; Meltzer CC, et al. Does cerebral blood flow decline in healthy aging? A PET study with partial-volume correction. 41: 1842-1848
(2) J Nucl Med 2001; Fazio F, Perani D. Importance of partial-volume correction in brain PET studies. 41: 1849-1850 (No abstract available)
(3) J Nucl Med 2001; Hoffman JM, et al. FDG PET imaging in patients with pathologically verified dementia. 41: 1920-28
(4) J Nucl Med 2001; Silverman DHS, Phelps ME. Evaluating dementia using PET: How do we put into clinical perspective what we know to date? 41: 1929-32 (No abstract available)
(5) J Nucl Med 1993; Henry T, et al. Clinical evaluation of interictal fluoring-18-fluorodeoxyglucose PET in partial epilepsy. 34: 1892-1898
(6) J Nucl Med 2001; O'Brien TJ, et al. The utility of a 3-dimensional, large field-of-view, sodium iodide crystal-based PET scanner in the presurgical evaluation of partial epilepsy. 42: 1158-1165
(7) J Nucl Med 2001; Derdeyn CP, et al. Comparison of PET oxygen extraction fraction methods for the prediction of stroke risk. 42: 1195-1197
(8) Semin Nucl Med 1992; Mazziotta JC, et al. The use of positron emission tomography in the clinical assessment of dementia. 22: 233-246
(9) Semin Nucl Med 1992; Volkow ND, Fowler JS. Neuropsychiatric disorders: Investigation of schizophrenia and substance abuse. 22: 254-267
(10) Semin Nucl Med 1992; Broich K, et al. Positron emission tomography in cerebral vascular disorders. 22: 224-232
(11) Semin Nucl Med 1992; Chungani HT. The use of positron emission tomography in the clinical assessment of epilepsy. 22: 247-252
(12) J Nucl Med 2001; Huang WS, et al. Evaluation of early-stage Parkinson's disease with 99mTc-TRODAT-1 imaging. 42: 1303-1308
(13) J Nucl Med 2001; Feigin A, et al. Metabolic network abnormalities in early Huntington's disease: an [18F]FDG PET study. 42: 1591-1595
(14) J Nucl Med 2001; Herholz K, et al. Direct comparison of spatially normalized PET and SPECT scans in Alzheimer's disease. 43: 21-26
(15) J Nucl Med 2002; Silverman DH, et al. Evaluating early dementia with and without assessment of regional cerebral metabolism by PET: A comparison of predicted costs and benefits. 43: 253-266
(16) Radiology 2003; Petrella JR, et al. Neuroimaging and early diagnosis of Alzheimer disease: a look to the future. 226: 315-336
(17) JAMA 2001; Silverman DH, et al. Positron emission tomography in evaluation of dementia. 286: 2120-2127
(18) AJR 2004; Norfray JF, Provenzale JM. Alzheimer's disease: neuropathologic findings and recent advances in imaging. 182: 3-13
(19) Radiology 2004; Patwardhan MB, et al. Alzheimer disease: operating characteristics of PET- a meta-analysis. 231: 73-80
(20) J Nucl Med 2004; Silverman DH. Brain 18F-FDG PET in the diagnosis of neurodegenerative dementias: comparison with perfusion SPECT and with clinical evaluations lacking nuclear imaging. 45: 594-607
(21) J Nucl Med 2005; Jeong Y, et al. 18F-FDG PET findings in frontotemporal dementia: an SPM analysis of 29 patients. 46: 233-239
(22) Seminars in Nuclear Medicine 1994, p.339
(23) Radiol Clin N Am 2004; Shiue CY, Welch MJ. Update on PET radiopharmaceuticals: life beyond flurodeoxyglucose. 42: 1033-1053
(24) Seminars in Nuclear Medicine, Oct. 1994, p.339
(25) J Nucl Med 2005; Drzezga A, et al. Prediction of individual clinical outcome in MCI by means of genetic assessment and 18F-FDG PET. 46: 1625-1632
(26) J Nucl Med 2005; CHen WP, et al. Rapid scanning protocol for brain 18F-FDG PET: a validation study. 46:1633-1641
(27) Radiol Clin N Am 2005; Newberg AB, Alavi A. The role of PET imaging in the management of patients with central nervous system disorders. 43: 49-65
(28) Radiol Clin N Am 2005; Silverman DHS, Alavi A. PET imaging in the assessment of normal and impaired cognitive function. 42: 67-77
(29) Radiol Clin N Am 2005; Newberg AH, Alavi A. PET in seizure disorders. 43: 79-92
(30) Radiol Clin N Am 2005; Fischman AJ. Role of [18F]-dopa-PET imaging in assessing movement disorders. 43: 93-106
(31) J Nucl Med 2006; Kobayashi M, et al. Diagnosis of misery perfusion using noninvasive 15O-gas PET. 47: 1581-1586
(32) J Nucl Med 2006; Mosconi L, et al. Hypometabolism exceeds atrophy in presymptomatic early-onset familial Alzheimer's disease. 47: 1778-1786
(33) J Nucl Med 2007; Ishii K, et al. Comparison of regional brain volume and glucose metabolism between patients with mild dementia with Lewy bodies and those with mild Alzheimer's disease. 48: 704-711
(34) J Nucl Med 2007; Lin TW, et al. Predicting seizure-free status for temporal lobe epilepsy patients undergoing surgery: prognostic value of quantifying maximal metabolic asymmetry extending over a specified proportion of the temporal lobe. 48: 776-782
(35) J Nucl Med 2007; Matsuda H. ROle of neuroimaging in Alzheimer's disease, with emphysis on brain perfusion SPECT. 48: 1289-1300
(36) J Nucl Med 2007; Nanni C, et al. 18F-DOPA PET and PET/CT. 48: 1577-1579
(37) J Nucl Med 2007; Inui Y, et al. Evaluation of probable or possible dementia with Lewy bodies using 123I-IMP brain perfusion SPECT, 123I-MIBG, and 99mTc-MIBI myocardial SPECT. 48: 1641-1650
(38) Radiology 2007; Hammoud DA, et al. Molecular neuroimaging: from conventional to emerging technologies. 245: 21-42