J Nucl Med 2000 Sep;41(9):1500-6
Evaluation of mammary lymphoscintigraphy by a single intratumoral injection
for sentinel node identification.
Valdes-Olmos RA, Jansen L, Hoefnagel CA, Nieweg OE, Muller SH, Rutgers EJ, Kroon
BB.
The aim of this study was to evaluate the findings of mammary lymphoscintigraphy
by a single intratumoral injection in 150 patients with breast carcinoma: 100
patients (group A) investigated in the validation phase of the study and 50
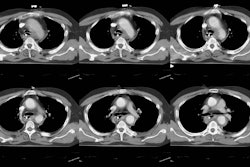
(group B) studied after the tracer dose was optimized. METHODS: Immediately
after injection of 99mTc-nanocolloid using a 25-gauge needle and a 0.2-mL
volume, simultaneous anterior and lateral images were acquired with a dual-head
gamma camera during 20 min followed by sequential static anterior and prone
lateral breast images after 30 min and after 2 and 4 h. 57Co-assisted skin
marking defined the sentinel node location for subsequent gamma probe, blue
dye-guided sentinel node biopsy. RESULTS: In group A (mean dose, 61.6 MBq;
range, 42-88 MBq) scintigraphy revealed lymph nodes in 83 patients (83%), with
an increase in the rate of visualization from 72% for the first 40 patients to
90% for the last 60; patient age (P = 0.01) and administered tracer dose (P =
0.04) were found to be significant factors for visualization, with optimal
results obtained from doses higher than 65 MBq. Lymph nodes were visible in 34
patients (41%) during the first 30 min after injection, whereas in 49 patients
appearance occurred at 2-4 h. A total of 97 lymphatic basins were visualized (80
axillary, 3 clavicular, 14 internal mammary). In group B (mean dose, 90.8 MBq;
range, 68-124 MBq), the visualization rate was 94%, with early lymph node
appearance in 27 patients (57%) and a total of 53 basins (45 axillary, 8
internal mammary). In combination with intraoperative blue dye mapping and y
probing, the identification rate increased to 90% in group A and 98% in group B.
Prone lateral images contributed to identification of intramammary lymph nodes
in a total of 14 patients and axillary nodes close to the injection site in 8
other patients. CONCLUSION: Mammary lymphoscintigraphy by single intratumoral
injection is a valid method for lymphatic mapping and identification of both
axillary and nonaxillary sentinel nodes. Lymph node visualization appears to be
improved with higher tracer doses. The compactness of the injection site enables
high-quality additional lateral images that can depict intramammary or axillary
lymph nodes adjacent to the injection site.