FDG Positron Emission Tomography in the Staging of Patients with Bronchogenic Carcinoma
General
Positron emission tomography (PET) relies upon actual physiologic information rather than morphologic features for the evaluation of bronchogenic carcinoma [74]. The most commonly used agent for PET tumor imaging is deoxy-glucose linked to 18-fluorine (a positron emitter). The agent 2-[F-18] fluoro-2-deoxy-D-glucose, or 18FDG, competes with glucose for facilitated transport into cells and also competes with glucose for phosphorylation by hexokinase. Unlike glucose, however, the phosphorylated form is not further metabolized and remains in the cell [75]. The agent is useful for imaging bronchogenic carcinoma because lung cancer cells have an increased cellular uptake of glucose due to an increased number of surface transport proteins and a higher rate of glycolysis in comparison to non-neoplastic cells [17,76,77].
Accurate preoperative staging of lung cancer is required to reduce the number of futile thoracotomies [159]. FDG PET imaging can have a significant impact on patient management by heightening suspicion for pulmonary malignancy, identifying unsuspected sites of disease, and by guiding selection of a biopsy site. Similarly, a negative PET scan indicates a low likelihood for malignancy and supports the use of conservative management and follow-up [136].
Increased glucose metabolism, however, is not completely specific for tumor [78] and can occur with infectious or inflammatory processes [79,132]. Similarly, lack of increased glucose metabolism does not necessarily exclude malignancy as carcinoid tumors [100] and bronchoalveolar cell carcinomas [101] may not demonstrate significant tracer uptake. Lesion detection on PET imaging depends primarily upon two factors: the amount of tumor uptake of 18FDG and tumor size [80].
PET-FDG for Staging of Bronchogenic Carcinoma
Although PET-FDG imaging has been used in differentiating benign from malignant pulmonary nodules, this discussion will focus on the use of PET imaging in the staging of bronchogenic carcinoma. Guidelines from the American Society of Clinical Oncology call for initial staging of lung cancer using CT of the chest and FDG imaging in the absence of distant metastases on the CT scan [169]. The American College of Chest Physicians also recommend PET imaging for the initial staging of non-small cell lung cancer [178]. Imaging with FDG is done in the fasting state to minimize competitive inhibition of FDG uptake by glucose (elevated glucose levels can result in decreased FDG tumor accumulation) [138]. Imaging while fasting also minimizes cardiac activity and improves detection of mediastinal metastases [139].
Unlike conventional imaging, FDG PET has the ability to define both local and distant disease and is a powerful imaging tool that can have tremendous impact on patient management. PET/CT has been shown to be more accurate in determining the correct TNM stage- 60% versus 40% for CT alone in one study [198]. Additionally, the combined use of CT and PET imaging may be cost effective for patient management [4]. A conservative strategy of using chest CT plus PET imaging has a potential cost savings of $1154 per patient [4,137]. This strategy would involve taking biopsy specimens from all positive findings with either CT or PET that might indicate non-resectable malignancy so that surgical candidates are identified more definitively [4,137]. The largest component of the cost savings realized by this approach results from prevention of unnecessary surgery in patients with unresectable disease [137]. Using this approach and assuming 85,000 patients (on the basis of national cancer statistics) undergo this diagnostic algorithm, the calculated savings would be $98,000,000 per year [139]. The discussion below will illustrate the role PET imaging plays in the TNM staging of non-small cell lung cancer.
Primary Tumor (T):
FDG PET imaging is of limited usefulness in determining the T status of the primary lesion [138]. Although tumor size can be estimated on PET imaging, this is best accomplished on CT scanning [137]. Additionally, PET scanning has limited accuracy in determining invasion into adjacent structures and for the detection of small satellite nodules [138,140]. One area in which FDG PET imaging is superior to CT scanning is in confirming a malignant effusion (T4 lesion) [131,154]. Malignant pleural effusion can be difficult to diagnose because cytologic evaluation is positive in only about two-thirds of cases [160]. The finding of increased FDG uptake greater than mediastinal blood pool activity that conforms to the pleural cavity is highly suggestive of a malignant effusion with an accuracy, of 80% to 92% [153,154]. The accuracy is slightly decreased as inflammatory or infectious pleural fluid collections can also demonstrate increased FDG accumulation [154,159].
Regional Lymph Node Metastases:
Conventional imaging:
Classification of lymph nodes on conventional CT imaging is based upon size. Mediastinal lymph nodes with a short axis diameter of greater than 1.0 cm are suspected of representing metastatic disease [152]. Unfortunately, up to 21% of nodes smaller than 1 cm are malignant and up to 40% of nodes larger than 1 cm are benign [152].
Exam interpretation:
Abnormal uptake in mediastinal or hilar nodes is typically defined as activity higher than the surrounding tissue uptake [141]. Standardized uptake values (SUV's) have been evaluated to determine if there is improved detection of lymph node metastases [181]. Using an SUV max of 2.5 is a reasonable threshold that results in acceptable sensitivity and specificity [181]. Quantification, however, poses a problem when determining activity on PET images in lymph nodes less than 1 cm in size because of the partial volume effects. This may falsely lower the SUV value [77] and visual assessment is generally as accurate (or more accurate for an experienced observer) as SUV determination [80,181]. Lymph nodes that contain calcification are more likely benign even if they demonstrate FDG accumulation [172].
Results:
Studies indicate that PET 18-FDG
imaging is superior to computed tomography and magnetic
resonance imaging in staging metastatic mediastinal lymph nodes
in patients with bronchogenic carcinoma [124,133,141,152,171].
PET imaging can contribute complementary non-invasive functional
information to the established size criteria for abnormal
mediastinal lymph nodes which improves the overall accuracy of
clinical staging for bronchogenic carcinoma [120]. Studies have
shown that 18FDG uptake within a normal sized node
is highly suggestive of metastatic disease [17,76,78,80,81] and
should be considered to represent malignancy until proven
otherwise [146]. A number of PET studies have also demonstrated
that the absence of 18FDG uptake in enlarged nodes
identified at CT is highly indicative of lack of metastatic
involvement [17,78,81,82].
In one study, the accuracy for staging mediastinal lymph nodes was 93% with PET/CT (compared to 63% for CT imaging) [152]. The use of PET/CT can result in a change in the planned treatment in up to 15% of patients [152]. In another study, PET/CT was significantly better than CT alone for nodal staging demonstrating improved accuracy and specificity [162]. Sensitivity rose from 70% for CT to 85% for PET/CT, specificity rose from 69% to 84%, and accuracy rose from 69% to 84% [162]. Overall staging was correct in 70% of patients by CT, and in 87% of patients by PET/CT [162]. Dwamena et al. performed a meta-analysis of 14 PET studies for staging mediastinal adenopathy and found an overall sensitivity of 79% (+/- 3%), and an overall specificity of 91% (+/- 2%) [124]. Accuracy was 92%, positive predictive value was 90%, and negative predictive value was 93% [124]. This is clearly superior to CT which has an overall reported sensitivity and specificity of 62% and 73%, respectively (using a transaxial short axis greater than 1.0 cm). PET staging of mediastinal nodes approaches mediastinoscopy which has reported sensitivities between 72% to 94% [141,181]. Results of the PET exam can also be used to more accurately guide mediastinal exploration with improved yield from preoperative mediastinal lymph node sampling [151]. The use of PET/CT may improve the sensitivity for the detection of mediastinal nodal metastases, but this may come at the expense of a reduced specificity (with a greater number of false positive cases) [179]. The number of false positive exams can be deceased by applying criteria regarding the attenuation density of the lymph node into image analysis [196]. Lymph nodes with tracer uptake greater than mediastinal blood pool activity, but showing high attenuation on CT (>70 HU) are considered by some authors to be benign (inflammatory or microscopic fibrotic reactive lymph nodes frequently show high attenuation on non-contrast CT) [196].
In T1 lung cancer:
The rate of mediastinal nodal metastases in patients with T1 lung cancer ranges from 16-23% [172]. In prospective study of patients with T1 lung cancer, the sensitivity of CT for mediastinal nodal staging has been reported to be only 27-41% [172]. In patients with T1 cancer, PET/CT can detect malignant nodal stations with a sensitivity of 47-56%, specificity of 100%, a positive predictive value of 100%, a NPV of 87%, and an accuracy of 88-90% [172,175]. Although this may seem low, CT imaging alone failed to identify 95% of proven malignant nodal stations [172]. All false negative PET/CT results were seen in nodes that were less than 10 mm [172].
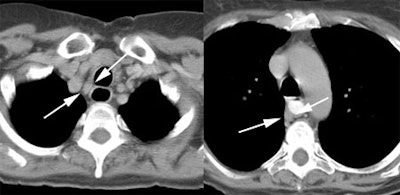
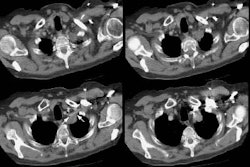
Example: This patient with a left lung non-small cell lung cancer demonstrated a pathologic aorto-pulmonary window node (N2) by CT size criteria (white arrow), and a non-pathologic retrocaval-pretracheal contralateral mediastinal node (N3) (yellow arrow). PET-FDG images revealed increased tracer accumulation within both nodes, consistent with metastases. (Case courtesy of H. Page McAdams MD, Department of Radiology, Duke University Medical Center)
|
NOTE: To load a higher resolution view, simply click directly on any of the images below. |
||
 |
 |
 |
Limitations of FDG PET in lymph node staging:
Although PET 18FDG imaging is clearly superior to helical CT for staging mediasitnal lymph nodes, it is not the "gold standard" for the confirmation or exclusion of N2/N3 disease in patients with NSCLC. False-negative examinations have been reported in association with both normal and enlarged lymph nodes that contained microscopic or small (under 5 mm) foci of tumor [17,76,79,80,129,133,140,142]. False-positive examinations have been reported in association with follicular hyperplasia [76,80,133], non-specific inflammation [81,83,129], epithelioid granulomas within nodes, pneumoconiosis [141], and anthracotic nodes [78,80,129,133]. Based upon these reports, a reduced specificity may be anticipated in populations with a higher incidence of granulomatous disease [141]. However, one observation has been that nodal groups containing calcification that demonstrate increased FDG uptake have a low likelihood for containing metastases [162]. On histopathologic analysis, these nodes contain areas of follicular hyperplasia, anthracotic pigmentation, and macrophage infiltration which may account for FDG uptake [162]. It may be reasonable to assume that FDG positive nodes containing calcification are benign [162]. Reactive nodes in patients with post-obstructive pneumonitis may also be expected to produce false-positive exams. Uptake in a thyroid nodule can be misinterpreted as supraclavicular adenopathy [140].
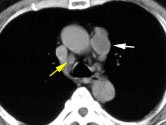
PET studies interpreted without
correlative anatomic imaging studies are less accurate, which
reflects the general problem with PET studies -- they suffer
from a lack of anatomic information [17,82]. Hilar nodes that
are in close proximity to the mediastinum can be mistakenly
classified as mediastinal nodes (false-positive
interpretation)-- especially in the right tracheobronchial and
subaortic region [17,133]. PET imaging can also be limited when
the primary lesion is central. Distinction between uptake in the
tumor and uptake in the adjacent hilar or mediastinal lymph
nodes may not be possible without the use of CT correlation and
even then the problem may not always resolved
[17,80,82]. Increased sensitivity and accuracy have been
demonstrated when PET image interpretation was combined with
correlative CT images [17,82].
|
A central cancer near the aortopulmonary
window, as in this case, is difficult to separate from
possible mediastinal lymph nodes. |
|
|
Despite the fact that some authors advocate that patients with negative 18FDG exams for pathologic mediastinal adenopathy should proceed to thoracotomy [74], such statements are premature. As previously discussed, false positive and false-negative exams occur with PET imaging. The reported positive predictive value of PET imaging for mediastinal staging has generally been reported to be between 74-93%, but can be as low as 45% [167]. The variability in false-positive exams suggests that PET-FDG results should not supplant histologic confirmation for suspected mediastinal nodal metastases [82,133]. For patients with stage II or III disease the incidence of false negative results is higher with PET than with mediastinoscopy (11.7% and 3%, respectively) [167]. Surgical studies have demonstrated that patients with metastases detected at mediastinoscopy have a worse prognosis than patients in whom N2 disease is found only at surgery [15,18]. Prospective studies have not been performed to determine whether patients with negative pre-operative 18FDG studies for mediastinal nodes have a prognosis similar to patients in whom N2 disease is found at thoracotomy following a negative mediastinoscopy. Therefore, mediastinoscopy will likely remain part of the standard protocol for mediastinal staging [167]. Pre-operative injection of FDG may help to guide intra-operative lymph node sampling [174].
Distant Metastatic Disease:
The presence of distant metastases
is classified as stage IV disease and generally precludes a
patient from curative surgical resection [167]. 18FDG
PET has significant potential to be used for detecting
extrathoracic metastases when whole body images are performed
[4,79,80,83,120]. Detection of unsuspected extra-thoracic spread
can be identified in 6% to 24% of patients (mean frequency of
about 13% [167]) and can significantly alter patient management
[80,106,120,133,140,141,143,144,151]. A 2013 meta-analysis demonstrated
a pooled sensitivity of 77% and specificity of 95% for the
detection of metastatic disease [215].
The likelihood for detecting unsuspected metastases increases with the patient's stage [167], but 11% of patients with stage I or stage II disease on conventional imaging can be found to have metastases [144]. In another study, 13% of patients with T1 non-small cell lung cancer had extrathoracic metastases at the time of diagnosis, and another 11% developed extrathoacic metastases within one year [157]. The likelihood for occult metastatic disease at presentation is also related to the type of cancer and can be found in up to 30% of patients with adenocarcinoma or large cell carcinoma, but is less common with squamous cell carcinoma (under 15% of patients) [167].
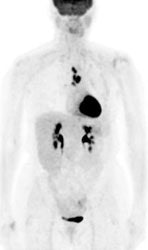
|
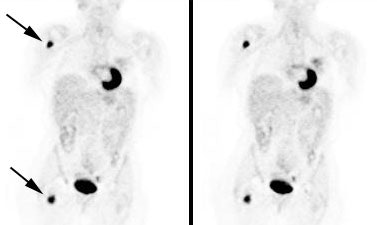
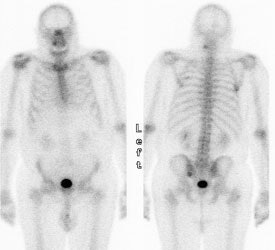
Unsuspected bone metastases: The patient shown below had a left lung non-small cell lung cancer (vaguely seen in the left lung on the PET images shown below). There was no uptake of tracer within the hila or mediastinum to suggest nodal metastases, however, unsuspected bone metastases were found in the right humerus and right hip (black arrows). These findings significantly altered patient management. |
|
|
|
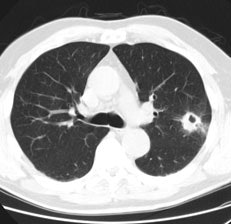
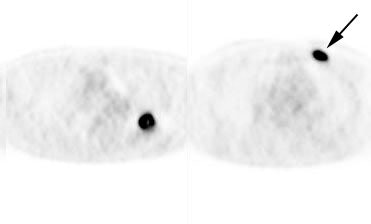
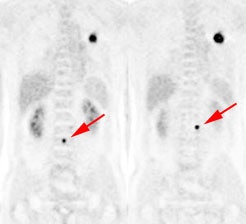
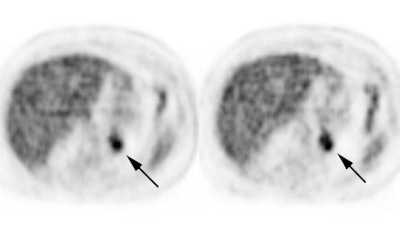
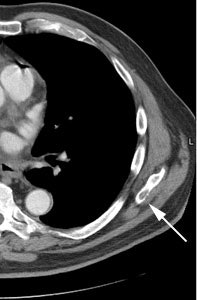
Unsuspected bone metastases: The patient shown below had a cavitary left lung non-small cell lung cancer. There was no uptake of tracer within the aortopulmonary window lymph nodes detected on CT to suggest metastases, however, unsuspected bone metastases were found in the left anterior 4th rib (black arrow) and lumbar spine (red arrows- not included in staging lung CT scan). The presence of bone metastases significantly alters patient prognosis and management. PET imaging provides a rapid whole body survey for the detection of unsuspected metastatic disease. |
|
|
Adrenal gland: One of the more common sites for metastatic disease is the adrenal gland. PET imaging can also be used to exclude abnormalitiy in sites of suspected metastatic disease on conventional imaging [140]- especially for indeterminate adrenal lesions [120]. An exam is generally considered positive for malignancy if uptake within the adrenal lesion is greater than or equal to the liver [158]. FDG PET has been shown to have a sensitivity 93% to 100% for the characterization of metastatic adrenal lesions in patients with bronchogenic carcinoma (specificity 80-100% and accuracy 92-100%) [135,147,158]. If FDG uptake is normal in an adrenal mass in a patient with NSCLC, then patients should be considered for curative resection [135]. However, false negative exams can occur with necrotic or hemorrhagic metastases and with small lesions [158]. Benign adrenal adenomas can have uptake of FDG equal to or greater than the liver resulting in a false positive exam [147]. A cutoff SUV of 3.1 has been shown to have a sensitivity of 97.3-98.5% and a specificity of 76-92% for characterization of malignant adrenal lesions [165,188]. Generally, however, adenomas demonstrate only mild tracer accumulation that is less than liver activity, but greater than background [147]. The use of PET/CT can improve characterization of adrenal masses by improving the exams specificity [165]. PET/CT permits further characterization of the lesion with an HU measurement of less than 10 indicative of a benign adrenal lesion, even if the lesion has SUV measurements greater than 3.1 [165,166,188].
|
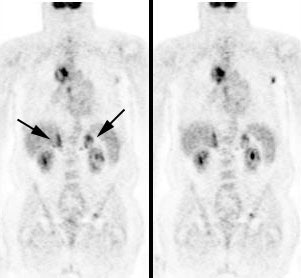
Bilateral adrenal metastases in a patient with non-small cell lung cancer: Uptake within the patients primary lung cancer can be seen within the right chest. Uptake within the bilateral adrenal glands (black arrows) confirmed the presence of adrenal metastases. |
|
|
|
Benign adrenal lesion with FDG uptake: The patient shown below had a left adrenal mass which had remained stable for 2 years (white arrow). The stability over time and CT features would be consistent with a benign adrenal lesion- likely an adenoma. Note the marked FDG uptake within the mass on PET imaging (black arrows). Benign adrenal adenomas can accumulate FDG resulting in false positive exams. The use of PET/CT has been shown to improve the specificity of the PET exam. |
|
|
Skeletal metastases: FDG PET has been shown to be superior to bone scan for the detection of skeletal metastases- PET sensitivity 92%, bone scan sensitivity 50% [146].
|
Widely metastatic non-small cell lung cancer to bone: The bone scan (left) significantly underestimated the extent of skeletal metastases as demonstrated on FDG PET imaging (right) which revealed multiple vertebral body metastases. Click PET image to view cine of patients PET scan (1.4 MB) |
|
|
Malignant pleural effusion: The results of fluid cytologic analysis have been reported to be positive for only 66% of malignant pleural effusions from NSCLC [167]. PET FDG has also been shown to be abnormal in patients with malignant pleural effusions [131]. Increased pleural FDG uptake is highly suggestive of a malignant effusion (sensitivity 95-100%, specificity 67-71%, and positive predictive value 63-95%) [131,167].
CNS metastases: Although PET imaging is overall superior to conventional imaging for detection of metastatic disease, PET should not replace conventional imaging for evaluation of brain metastases [120,141,170]. The normal brain has substantial glucose uptake and metastatic foci are difficult to detect on PET FDG images [120,141,146,170]. In a meta-analysis of prospective studies, PET had a pooled sensitivity of only 21% for the detection of CNS metastatic disease, compared to 77% for MRI [215]. In general, PET imaging of the brain does not provide additional clinical information regarding the presence of metastatic disease in lung cancer patients [170].
False positive examinations for metastatic disease have been described [130,133,135,142,143]. As a result, a positive PET scan cannot be accepted as definitive proof of metastases and further staging procedures are usually required so that patients are not denied potentially curative surgery [130,133]. Of note, in one study a patient classified as having stage IV disease based upon the presence of a liver metastasis on PET imaging initially had a normal CT exam of the liver [130]. A follow-up CT exam revealed a metastatic lesion corresponding to the original PET abnormality [130]. This indicates that the initial CT was actually a false negative exam and that PET may be more sensitive than conventional modalities for detection of certain metastatic lesions [130].
Secondary primary malignancy:
PET imaging can identify a second primary malignancy or
pre-malignant lesion in about 3% of patients with NSCLC [215].
Patient Staging/Management:
In the prospective evaluation of the
utility of FDG PET for the primary clinical staging of patients
presenting with non-small cell lung cancer, PET findings
resulted in a different stage than the one arrived at by
convention methods in 27% to 61% of patients
[133,140,141,144,204]. Generally, FDG PET exam findings reveal
more extensive disease than was suspected clinically- thereby
reducing the likelihood of expensive non-curative surgery in
lung cancer patients [144,151,204]. This has a great impact on
patient management decisions [204]. FDG PET exam results can
change or influence patient management decisions in 35% to 67%
of patients [140,141,144,204]. PET imaging as part of the
preoperative staging has been shown to reduce the number of
unnecessary surgeries (up to 51% relative reduction in futile
thoracotomies [215]) [206]. Additionally, the PET/CT stage is
more strongly predictive of overall survival compared to
conventional staging [204].
A study by Seltzer et al. examined the impact PET exam results had on patient management by sending a questionnaire to physicians that had referred patients with known or suspected lung cancer for FDG imaging [150]. The FDG exam findings resulted in a change in patient stage in 44% of cases (29% upstaged, 15% down-staged) [150]. In this same study, the planned modality for treatment was changed in 39% of patients based upon the PET exam results [150]. A prospective multicenter study FDG PET imaging in patients deemed to be surgical candidates by conventional imaging revealed unresectable disease in 14% of patients [171]. In a separate prospective, randomized trial, FDG PET imaging was also shown to decrease the number of futile thoracotomies (defined as surgery for a benign lesion, N2 nodal disease detected at mediastinal dissection, stage IIIB lesion, or death from any cause within one year) [151]. For patients with conventional workups (CWU), futile thoracotomy occurred in 41% of patients [151]. In patients that underwent CWU plus PET imaging, futile thoracotomy occurred in 21%- a 51% reduction from CWU alone [151]. In another prospective study, PET-CT was again shown to reduce the number of futile thoracotomies (from 52% with CWU to 29% in the PET-CT group) [191]. In this study, for every 5 PET-CT scans, one futile thoracotomy was avoided [191]. Unfortunately, PET-CT did not appear to affect overall mortality [191].
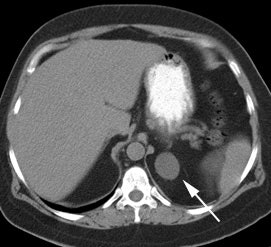
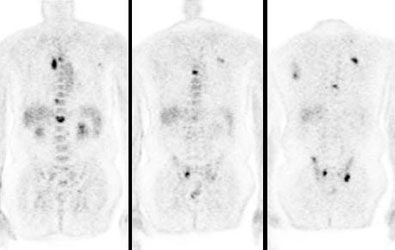
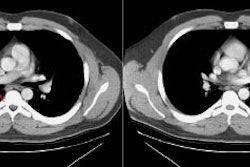
|
Change in stage: The patient below was felt to have Stage IIIB disease based upon the chest CT findings. FDG PET imaging confirmed ipsi- and contralateral mediastinal adenopathy, but also reveal a left scapular metastasis (seen retrospectively on the CT scan [white arrow]). A left iliac metastasis was also identified (black arrow right PET image). This resulted in a change in patient stage as the patient was now has Stage IV disease. |
|
|
van Titeren et al performed a randomized trial to compare conventional staging work up (CWU), to a staging workup that included FDG PET (CWU+PET) imaging. The study group included patients with suspected or proven non-small cell lung cancer. Patients were considered to have undergone a futile thoracotomy if the lung lesion proved to be benign, there was pathologically proven mediastinal lymph node involvement, or if the patient experienced recurrent disease or death from any cause within one year after randomisation. All potential sites of nodal or distant metastases which might have a major effect on patient management were confirmed by other means. Unconfirmed PET findings were ignored. Prior to surgery, PET imaging identified nearly twice as many patients (32 patients) with unresectable disease compared to CWU (18 patients). They found that a significantly greater number of patients in the CWU group (41%) underwent futile thoracotomy compared to the CWU+PET group (21%). Assessment of resectability by CT and PET was discordant in one-third of cases, and the PET exam was correct in two-thirds of these instances. PET imaging also helped guide preoperative mediastinal lymph node staging. The yield of preoperative node staging was 63% in the CWU group, compared with 83% in the CWU+PET group. Unsuspected distant metastases were identified in the CWU+PET group in 8% of patients. The addition of PET to conventional workup can strikingly reduce the number of futile thoracotomies in patients with suspected potentially resectable non-small cell lung cancer. It's main advantage is to upstage patients, alleviating unnecessary surgery and directing appropriate medical therapy.
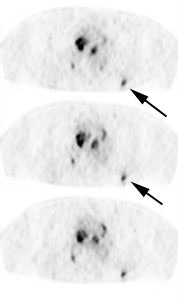
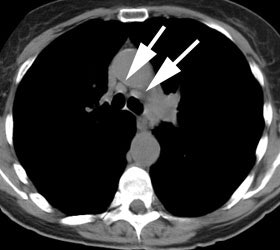
|
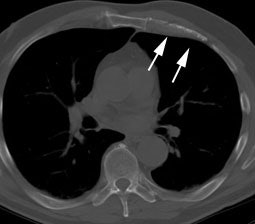
Futile thoracotomy- extensive mediastinal lymph node metastases: The patient below had a T1 lesion in the left lower lobe (black arrow). Pre-operative CT scan revealed lymph nodes within the mediastinum which were not pathologic by size criteria (white arrows). The patient underwent thoracotomy for tumor resection and was found to have positive hilar lymph nodes- a mediastinal node dissection was not performed. A post operative PET scan revealed extensive mediastinal lymph node metastases to the normal sized nodes. Had PET imaging been done pre-operatively, thoracotomy could have been avoided in this patient. |
|
|
However, PET findings should not be used in isolation without clinical, other imaging, or histologic data [142]. Up to 10% of patients classified as non-surgical candidates based upon FDG PET exam findings have been shown to have a lesser stage at surgery. Note however, that in this same study CT inaccurately classified 32% of patients as non-surgical [142] and PET has been shown to be substantially more accurate than CT in almost all comparative studies [144].
The spatial resolution of PET is generally insufficient to exclude small-volume disease [144] and FDG PET imaging can underestimate disease extent [142]. Up to 13% of patients classified as surgical candidates based upon their PET exam have been shown to have more advanced disease histologically (in this same study CT incorrectly classified 19% of patients with advanced disease as surgical candidates) [142].
In summary:
FDG PET imaging is a very useful complementary imaging modality to conventional methods for the clinical staging of patients with NSCLC. The combined diagnostic value of PET and CT is superior to either study alone [179]. FDG PET imaging improves the overall accuracy of clinical staging for bronchogenic carcinoma through better identifications of nodal and distant metastases. In doing so, PET imaging has been shown to have a significant impact on patient management by better identifying those patients that will most benefit from primary surgical treatment. Similar to conventional imaging, PET suffers from both false-positive and false-negative exams. Additionally, PET imaging alone cannot replace the structural information provided by standard anatomic imaging techniques. Bronchial wall, pleural, and vascular invasion are difficult to image with PET and from a surgical perspective, an anatomical image remains necessary for operative planning [84]. With the use of high quality PET/CT imaging, however, all of this information can be acquired in a single imaging session.