Pulmonary Pseudotumor: (Plasma Cell Granuloma or Inflammatory myofibroblastic tumor)
Clinical:
Pulmonary pseudotumor represents an uncommon, non-neoplastic, occasionally aggressive process that may begin as an organizing inflammatory process- possibly an organizing pneumonia in patients with a subclinical infection. The lesion has also been referred to as a plasma cell granuloma, inflammatory myofibroblastic tumor, fibroxanthoma, xanthomatous pseudotumor, and plasma cell-histiocytoma complex. It can be seen at any age, but almost half the cases are found in patients under the age of 20 years. In fact, it is the most common "tumor-like" lung lesion described in patients under 16 years of age. The lesion has no sex predilection [4]. Up to 60% of affected patients can be symptomatic with non-specific pulmonary symptoms such as cough, fever, dyspnea, chest pain, or hemoptysis. ABout 20% of patients have an antecedent pulmonary insult- usually infection [4]. Typically the lesion does not grow or regresses, but slow growth can be seen and mimic a malignant lesion. Most lesions are surgically resected as a neoplasm is difficult to exclude. The lesion itself has no malignant potential [1].X-ray:
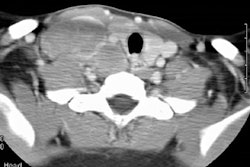
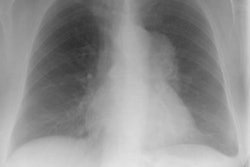
The lesion is usually a well-defined, peripheral solitary mass lesion (87% of cases) from 1 to 10 cm in size most commonly in the lower lobes (up to 60% in one study [1]). The lesion may have calcification (15%) especially if the mass is large and calcification may be more common in children [1]. Pleural effusions (typically small and ipsilateral) can be found in up to 13% of cases. Mediastinal or tracheo-bronchial disease is not typically associated with the lesion, but local invasion of these structures has been described [1]. Multiple nodules (5%) are rare and endobronchial lesions constitute about 10% of cases [4]. Pseudotumor may rarely cavitate (5%). Lymphadenopathy is rare [4].On CT the lesion is usually a well marginated, lobulated mass, of heterogeneous attenuation, with variable contrast enhancement. On the very small number of lesions studied with MR the lesion has had heterogeneous signal intensity slightly greater than skeletal muscle on T1 images, high signal intensity on 2 images, and diffuse, heterogeneous enhanacement with gadolinium.
REFERENCES:
(1) Radiology 1998; Agrons GA, et al. Pulmonary inflammatory pseudotumor: Radiologic features. 206: 511-518
(2) Curr Probl Diagn Radiol 1996; 25(3): May/June
(3) Radiographics 2002; Gimenez A, et al. Unusual primary lung tumors: a radiologic-pathologic overview. 22: 601-619
(4) Radiographics 2003; Narla ND, et al. Inflammatory pseudotumor. 23: 719-729