Pleuropulmonary blastoma: a clinicopathologic study of 50 cases.
Priest JR, McDermott MB, Bhatia S, Watterson J, Manivel JC, Dehner LP
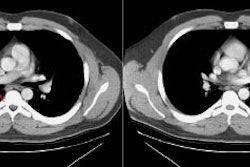
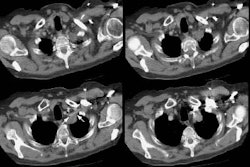
BACKGROUND: Pleuropulmonary blastoma (PPB) is a unique dysontogenetic neoplasm of childhood that appears as a pulmonary and/or pleural-based mass and is characterized histologically by a primitive, variably mixed blastematous and sarcomatous appearance. METHODS: Histologic material from all cases was reviewed and the tumors subclassified as type I (purely cystic), type II (cystic and solid), or type III (purely solid). Data regarding presenting symptoms, family history, operative findings, pathologic subtypes, therapeutic interventions, and outcome were correlated with survival by standard statistical methods. RESULTS: The series was comprised of 24 males and 26 females. Respiratory difficulty with or without fever was the most common clinical symptom reported. Cyst formation in the affected lung was identified radiographically in 19 children (38%) at or before the definitive pathologic diagnosis. The ages at presentation of the 7 type I, 24 type II, and 19 type III PPBs were significantly different: 10, 34, and 44 months, respectively (P < 0.001). Local recurrence developed in 1 of 7 type I PPBs (14%) and in 18 of 43 type II and III PPBs (46%); distant metastasis occurred in 13 patients, chiefly to the brain/spinal cord or bone, and was observed only in those with type II or type III PPB. Patients with pleural or mediastinal involvement fared significantly worse than those without such involvement. Five-year survival was 83% for type I and 42% for types II and III. Survival differences on the basis of pathologic subtype did not reach statistical significance. CONCLUSIONS: PPB is an aggressive, intrathoracic neoplasm of early childhood with an unfavorable outcome. Although survival differences among patients with different histologic subtypes of disease did not reach statistical significance, the apparently better outcome for patients with purely cystic type I tumors may be borne out in a large series. These observations support the premise that type I and III PPB are bridged morphologically by type II PPB with its combined cystic and solid features. The PPB should be regarded as the pulmonary dysontogenetic analogue to Wilms' tumor in the kidney, neuroblastoma in the adrenal gland, and hepatoblastoma in the liver. Molecular genetic investigations, especially in constitutional PPB, should be revealing. In view of the poor outcomes for patients with types II and III, new and aggressive therapies must be developed.