In 1999 Dr. Susan Leech and colleagues at John Radcliffe Hospital in Oxford, U.K., published an x-ray scoring system for assessing childhood defecation disorders. The Leech method consists of a point scale of 0-5 in three areas of the colon:
- Ascending colon and proximal transverse colon
- Distal transverse colon and descending colon
- Rectosigmoid
A score of 0 indicates no stool while a score of 5 means gross fecal loading with bowel dilation. The total score can range from 0-15. In their paper in Pediatric Radiology, the authors declared the scoring system to be "a clinically useful and a reproducible tool in assessing childhood constipation" (April 1999, Vol. 29:4, pp. 255-258).
Six years later, does the Leech system continue to be useful? Yes and no, according to two more recent studies out of the Netherlands. The authors of both studies concur that a simplified approach to evaluating fecal load on abdominal x-ray is required. But while one group gave the Leech method their vote of confidence, the other found it to be of limited value.
Leech, Barr, Blethyn
In the first paper, Dr. Maurice van den Bosch and co-authors pointed out that the most thorough objective test for assessing constipation in children is also the most tedious -- weighing stool requires daily samples, and measuring whole-gut transit time (also known as colonic transfer time or CTT) calls for multiple abdominal radiographs over a five-day period.
A one-time x-ray is less expensive and safer, they stated, but no common policy is in place for how these films should be reviewed. To that end, the group compared three different scoring systems for fecal retention assessment on a single radiograph.
"Although the diagnostic accuracy of these methods has been evaluated, their reproducibility has never been properly determined," the group wrote in Pediatric Radiology online (January 18, 2006).
The authors are from the University Medical Center and Wilhelmina Children's Hospital, both in Utrecht.
Forty x-rays from 40 children (mean age 7) were selected for this retrospective study. The images were reviewed by two pediatric radiologists during two sessions, six weeks apart. Besides the Leech method, each radiograph was scored according to two other systems:
- The Barr method quantifies the amount and consistency of feces in the ascending colon, transverse colon, descending colon, and rectum (Clinical Pediatrics, November 1979, Vol. 18:11, pp. 674-679).
- The Blethyn method evaluates the amount of feces in the large bowel (Archives of Diseases of Childhood, December 1995, Vol. 73:6, pp. 532-533).
Kappa coefficients were calculated as indications of intraobserver and interobserver variability.
According to the results, the Leech method showed the highest reproducibility with high intraobserver agreement for the first observer (0.88) and the second (1.00). There was also interobserver agreement -- 0.91 in the first session and 0.84 in the second.
Agreement using the Barr method was fair and agreement was low for the Blethyn scoring system, the authors reported. Van den Bosch's group concluded that the Leech method was useful for the systematic quantification of constipation.
'One-shot observation'
As time-consuming as it may be, measuring CTT does offer the most precise and consistent way to glean information about colorectal motor function in defecation disorders, according to Dr. Fleur de Lorijn, Ph.D., and colleagues from two Dutch institutions. Using the Leech method on a single plain abdominal x-ray may offer a convenient "one-shot observation," but it may not necessarily be reliable.
"The degree of fecal loading fluctuates daily and depends on food intake, the will of the child to defecate, and whether or not the child went to the toilet just before the abdominal radiography was taken," the authors wrote (Pediatric Radiology, January 2006, Vol. 36:1, pp. 43-49).
De Lorijn's group is from Emma Children's Hospital and the Academic Medical Centre, both in Amsterdam.
For this study, 52 patients were included (mean age 9 years). They were diagnosed with either functional nonretentive fecal incontinence (FNRFI) or functional abdominal pain (FAP). These children ingested one capsule with 10 radiographic opaque markers a day over a six-day period to determine the CTT. The control group was made up of children who had clinical characteristics of FNRFI or FAP but no fecal loading on x-ray.
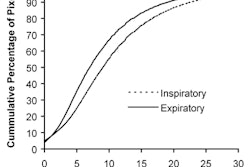
Using the Leech method, the same x-ray was reviewed and scored by a senior radiology resident, a pediatric radiologist, and a pediatric gastroenterologist. The radiograph was scored again four weeks later. The CTTs were assessed once by de Lorijn. Sensitivity and specificity were judged with a receiver operator characteristics (ROC) plot; the area under the ROC curve (AUC) was used as the indicator of diagnostic accuracy.
 |
| The Bouchoucha method was used to determine CTT. Here, the day 7 radiograph was used to count the number of markers visible in the colon. The number of markers multiplied by 2.4 produced the total CTT hours. A CTT of more than 62 hours was considered delayed. The Leech method scoring method was applied to the right colon, the left colon, and the rectosigmoid segment. Image courtesy of Dr. Fleur de Lorijn, Ph.D. |
The results showed that measuring CTT had better overall accuracy, turning in an AUC of 0.90 compared to 0.68 for the Leech method. The sensitivity for the Leech method was 75%, while the sensitivity for CTT was 79%. The specificity for Leech was 59% versus 92% for CTT. The positive predictive value for Leech was 72% versus 69% for CTT, and the negative predictive value was 63% for Leech and 97% for CTT.
The authors wrote that they found significant intraobserver variability for reader one (p = 0.005) and reader two (p < 0.001). There was no significant difference for the third reader. However, in terms of interobserver variability, reader three did score consistently lower than readers one and two.
"History and physical examination remain the cornerstone in the diagnostic workup of children with functional gastrointestinal disorders," the authors concluded. The large intraobserver and interobserver variability between the readers, as well as the low diagnostic accuracy, make the Leech method unreliable in this patient population.
In an e-mail interview with AuntMinnie.com, de Lorijn shared more details about how childhood constipation is dealt with at her institution.
At your institution, do these patients routinely undergo CTT or is there a set of criteria that they must first meet (based on history/physical exam) before moving on to imaging?
At our institution, our patients do not undergo routinely a CTT. Constipation is a clinical diagnosis! If differentiation between constipation and solitairy encopresis is difficult then a CTT measurement is a good diagnostic tool. Solitairy encopresis shows always a normal CTT (< 62 hours). Furthermore, if rectal examination is not possible or if you do not trust the child's diary, then you can perform a CTT to objectify the complaints.
Could there be a role for a single x-ray and the Leech method as a screening tool to determine if patients should go on to more invasive imaging?
As I mentioned before, in our opinion constipation is a clinical diagnosis, meaning that we only perform an x-ray in the above mentioned situations. More invasive imaging is mostly not necessary. In some children we perform barostat procedures, and in a very small group we perform duodenal/colonic manometries. This is mainly to evaluate or get new insights in the pathophysiology of constipation.
The study by van den Bosch and colleagues on the Leech method had results that differed from yours with regard to observer variability. Any thoughts on their study and why their outcome was different?
I'm not sure why our results are different. They used two observers instead of three. They used two pediatric radiologists; we used one pediatric radiologist, a general radiologist, and a pediatric gastroenterologist.
In general practice, I think that mainly general radiologist will evaluate these x-rays. Furthermore, it is possible that the patient groups included are different. Patients with severe complaints (defecation frequency of less than twice a week, etc.) will show more severe impaction on a x-ray. I think that x-rays of patients with severe complaints will be easier to evaluate than patients with minor complaints.
Do you think there is any role for colonoscopy and/or virtual colonoscopy, instead of x-ray, for assessing constipation in children?
I don't think that there is any role for colonoscopy or virtual colonoscopy for assessing constipation in children. Too invasive (colonoscopy) and too expensive. History, physical examination and a diary is in most cases enough to diagnose constipation.
By Shalmali PalAuntMinnie.com staff writer
March 17, 2006
Related Reading
VC earns high marks in symptomatic kids, July 7, 2005
Abdominal radiography not useful in constipated children, July 14, 2005
Test predicts ongoing constipation in kids, August 24, 2004
Copyright © 2006 AuntMinnie.com