The epidemiological emphasis in osteoarthritis (OA) has shifted from the incidence of the disease to identifying its risk factors. Among rheumatologists, OA is gaining acceptance as a multisymptom disorder that ultimately leads to a similar clinical and pathological end point. But questions remain as to the role that imaging plays in tracking the OA path.
In a paper in Best Practice & Research Clinical Rheumatology, Dr. Jolanda Cibere, Ph.D., offered her thoughts on the value of x-ray -- and to some degree MRI -- in OA. More specifically, she stated that the routine use of plain radiography in OA patients was not indicated, although it has been the primary diagnostic modality for OA for many decades.
"The usefulness of plain radiography in the diagnosis of OA relates not only to its ability to detect disease, but also depends on the definition used to determine whether disease is present," wrote Cibere, who is an assistant professor of medicine at the Arthritis Research Centre of Canada, University of British Columbia in Vancouver. "The radiographic evaluation (has) three purposes ... to establish the diagnosis or severity of OA ... to monitor disease activity ... and to look for complications" (Best Practice & Research Clinical Rheumatology, February 2006, Vol. 20:1, pp. 27-38).
How successfully x-ray lives up to its purpose depends on how it's used and whether its limitations can be overcome, Cibere stated.
OA signs on x-ray
The radiographic features of OA include osteophytes and joint-space narrowing (JSN). If cartilage degeneration is severe enough, it will manifest on x-ray as decreased distance between opposing articular bony surfaces, Cibere wrote.
Osteophytes are considered a hallmark of OA, but clinical signs may not correlate precisely with x-ray. Cibere noted that in distal interphalangeal joints, osteophytes were only seen 49.7% of the time on x-ray although they were all found on clinical exam, according to a previous study (Annals of the Rheumatic Diseases, April 1998, Vol. 57:4, pp. 246-248).
 |
| Rapidly destructive hip osteoarthritis in 68-year-old woman with right-sided hip pain. Anteroposterior radiograph obtained at onset of symptoms shows moderate superolateral joint-space narrowing and small subchondral cystic lesion in acetabulum. Boutry N, Paul C, Leroy X, Fredoux D, Migaud H, Cotton A, "Rapidly Destructive Osteoarthritis of the Hip: MR Imaging Findings" (AJR 2002; 179:657-663). |
For JSN, weight bearing is an important component of x-ray evaluation, especially in the hips and knees. As a result, the standard patient position has been standing and bilateral weight bearing, but this protocol does benefit from refinement. Cibere suggested that in hip OA, the oblique standing view offers a better view of JSN. In knee OA, she endorsed the semiflexed view, which brings more of the posterior femoral condyle into the picture.
MRI for OA
When x-ray isn't sensitive enough to offer a clear picture of the disease process, MRI may fill in the gaps. For example, osteophytes overlapped by adjacent anterior and posterior bony features may remain undetected on x-ray, but can be found with MRI. Cibere cited a 2003 study in which 58 subjects with knee pain had normal x-rays while MRI turned up cartilage defects ranging from more than 50% to full thickness. They would have remained undiagnosed without the MR exam, she pointed out (Osteoarthritis and Cartilage, June 2003, Vol. 11:6, pp. 387-393).
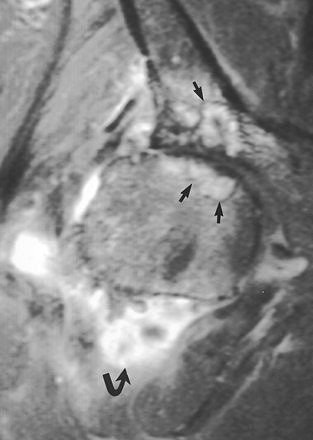 |
| Rapidly destructive hip osteoarthritis in 68-year-old woman with right-sided hip pain. Coronal fat-suppressed gadolinium-enhanced T1-weighted MR image (TR/TE, 720/20) obtained six months after onset of symptoms shows frank synovitis (curved arrow). Note presence of cystlike subchondral defects (straight arrows) at weight-bearing surfaces of femoral head and acetabulum. Boutry N, Paul C, Leroy X, Fredoux D, Migaud H, Cotton A, "Rapidly Destructive Osteoarthritis of the Hip: MR Imaging Findings" (AJR 2002; 179:657-663). |
For JSN assessment, MRI can reveal meniscal degeneration, which is a key to accurate JSN measurements. A study by radiologists at the Boston VA Medical Center showed that increasing meniscal subluxation on MRI correlated strongly with the severity of JSN on plain x-ray in the symptomatic knee (Osteoarthritis and Cartilage, November 1999, Vol. 7:6, pp. 526-532).
In keeping with the new clinical approach that stresses OA tracking, Cibere acknowledged that MRI can detect degenerative changes at an earlier stage than x-ray. But as is usually the case with the modality, the high cost of MR is a limiting factor for its use in OA, she said.
Future of OA imaging
"Ultimately, the performance of a diagnostic test in clinical practice is only warranted if the result -- normal or abnormal -- will have an effect on the management of the patient," Cibere wrote. So if x-ray cannot be recommended as part of routine OA workup, then when should it be employed?
Currently the best use for x-ray is to rule out conditions other than OA, according to Cibere. The three clinical reasons for obtaining x-ray are acute severe pain, pain with locking, and/or persistent unexplained joint pain. If x-ray turns up nothing abnormal, then additional tests, such as MRI or arthroscopy, might be warranted, she said.
Down the road, OA radiographic protocol will need to be improved to deal with some of the modality's major pitfalls -- a tendency to underestimate the amount of JSN, and a tendency to over- or underestimate disease progression.
Also, Cibere called for more sophisticated clinical reporting and scoring systems. The most commonly used system, Kellgren-Lawrence, uses a global score of 0-4 to grade osteoarthritic joints. But Kellgren-Lawrence suffers from ambiguity, especially between grade 0 (no OA) and grade 1 (doubtful OA). Another reporting option is the Altman atlas, which can be applied to JSN in particular. However, this system can be problematic because it applies grades only to individual features of OA.
"It is not clear which individual or combination of features should be used to define radiographic OA," Cibere explained. Finally, there is a lack of specificity to descriptive assessments of OA (mild, moderate, severe) in other radiological reporting systems.
Cibere called for "the development of algorithms and guidelines for the use of plain radiography in patients with chronic joint pain." Future research will need to focus on two issues: a better clinical definition of OA, which might negate the need for x-ray altogether, and/or a reduction in the discord between clinical symptoms and changes seen on x-ray, she stated.
By Shalmali Pal
AuntMinnie.com staff writer
March 31, 2006
Related Reading
Meniscus damage contributes to cartilage loss in knee osteoarthritis, March 10, 2006
Subchondral bone marrow edema common in knee osteoarthritis, March 8, 2006
Copyright © 2006 AuntMinnie.com