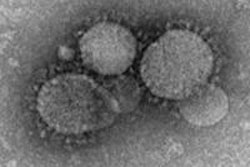
Research from Saudi Arabia, the epicenter of the Middle East respiratory syndrome coronavirus (MERS-CoV), underlines how imaging investigations can help early detection and management of disease progression, thereby playing a crucial role in predicting patient outcome and preventing the spread of infection.
Increased awareness of MERS-CoV and building an understanding of early chest radiographic features of this deadly new viral infection can improve early segregation of affected patients from those with other common infections, reducing its spread in the community. The researchers also assert that chest radiographic scores and CT lung scores provide information vital to care strategy and patient prognosis.
Because Saudi Arabia has experienced heavy losses from MERS-CoV, a group led by Dr. Karuna M. Das conducted a retrospective study of 55 patients with confirmed MERS-CoV infection admitted to King Fahad Medical City Hospital in Riyadh, where Das was working as a consultant cardiovascular and thoracic radiologist at the time.
 Frontal chest radiograph shows bilateral ground-glass opacities at initial presentation of the disease. All images courtesy of Dr. Karuna M. Das.
Frontal chest radiograph shows bilateral ground-glass opacities at initial presentation of the disease. All images courtesy of Dr. Karuna M. Das.According to their previous research, Das and colleagues found 83% of initial chest x-rays showed lung parenchymal abnormalities in MERS-CoV. The main chest x-ray finding associated with MERS-CoV was ground-glass opacity (image above) in 66% of cases, followed by consolidation in 18%. Both ground-glass opacity and consolidation were apparent in 16% of cases. Less common radiographic findings included irregular linear-type airspace disease (9%) and multicentric cavitation (2%). The main findings can be seen in the two tables below.
| Radiological abnormality visualized at initial x-ray | Findings in 55 patients (in %) |
| No abnormality | 17 |
| Abnormality | 83 |
| Ground-glass opacity | 66 |
| Consolidation | 18 |
| Ground-glass opacity & consolidation | 16 |
| Linear-type airspace disease | 9 |
| Multicentric cavitation | 2 |
Quantitative results
In the paper published online on 21 March 2016 and scheduled to appear in the June edition of the American Journal of Roentgenology (June 2016, Vol. 206:6, pp. 1-9), the authors also described how quantitative evaluation of sequential chest x-rays in severely ill patients in the intensive care unit (ICU) can be used to predict a poor prognosis and higher mortality in MERS-CoV patients.
The mean chest radiographic score was significantly higher in patients who died than in those who recovered (13.0 ± 2.6 versus 5.8 ± 5.6, p = 0.001). Furthermore, a higher association rate of the following features was seen in patients who died than in those who recovered: pleural effusion (63% versus 14%, p = 0.001), type 4 radiographic progression (63% versus 6%, p = 0.001), and pneumothorax (47% versus 0%, p = 0.001), according to the authors. They stressed the need for careful and early identification of these prognostic chest x-ray findings in MERS-CoV-infected patients.
"The presence of type 4 radiographic deterioration pattern, pleural effusion, and pneumothorax were predictors of imminent danger requiring most active intervention and treatment," Das said in an interview.
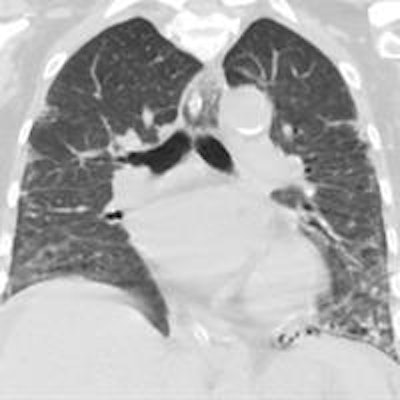
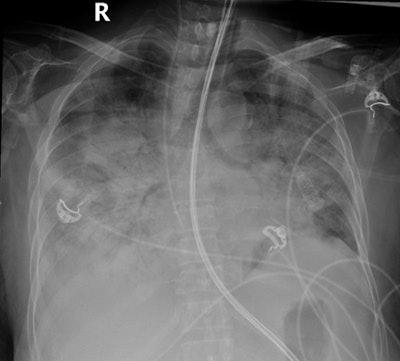 Above: Frontal chest radiograph performed when the patient was admitted with adult respiratory distress syndrome to the ICU. The x-ray shows bilateral extensive airspace disease with ground-glass opacities and consolidation (chest radiographic score 18). Below: Coronal section of a chest CT reveals early depiction of bilateral peripheral multiple ground-glass opacities in both lung fields.
Above: Frontal chest radiograph performed when the patient was admitted with adult respiratory distress syndrome to the ICU. The x-ray shows bilateral extensive airspace disease with ground-glass opacities and consolidation (chest radiographic score 18). Below: Coronal section of a chest CT reveals early depiction of bilateral peripheral multiple ground-glass opacities in both lung fields.Early detection of ground-glass opacities in CT compared with chest x-rays and CT lung scores also are useful tools in detecting infection and evaluating disease progression and patient prognosis. The mean CT lung score of those who died (15.78 ± 7.9) was significantly higher than those who completely recovered (7.3 ± 5.7) (p = 0.003), Das and colleagues noted.
| Relationship of pleural effusion with other variables in 55 patients with MERS-CoV | |||
| Variables | Pleural effusion (n = 17) | No pleural effusion (n = 38) | P-value |
| Age (y), mean ± SD (standard deviation) | 52.6 ± 17.8 | 44.2 ± 15.0 | 0.08 |
| Male sex, no. (%) of patients | 5 (29.4) | 11 (28.9) | 0.97 |
| Healthcare workers, no. (%) of patients | 2 (11.8) | 20 (52.6) | 0.004 |
| No. of comorbidities, mean ± SD | 2.0 ± 1.2 | 1.6 ± 1.0 | 0.06 |
| Percentage of lung involvement at peak of MERS-CoV infection, mean ± SD | 11.5 ± 3.0 | 6.8 ± 6.0 | 0.001 |
| No. (%) of patients who died | 12 (70.6) | 7 (18.4) | 0.001 |
Initial findings overlooked
Startlingly, the researchers noticed in many cases that radiological signs of infection in patients coming to the hospital from risk areas had been overlooked, and the seriousness of the disease process had been underestimated. These patients were sent home only to return several days later when their condition had drastically worsened or developed into adult respiratory distress syndrome (ARDS) -- and after they had potentially infected others. In this category of outpatients, the mortality rate from ARDS was higher than in those kept and monitored at the hospital.
 Dr. Karuna M. Das now works as a consultant thoracic and cardiovascular radiologist at UAE University in Al Ain, United Arab Emirates (UAE).
Dr. Karuna M. Das now works as a consultant thoracic and cardiovascular radiologist at UAE University in Al Ain, United Arab Emirates (UAE)."After a patient undergoes chest radiography, typically a radiology resident will read and report the image three to six hours later, and the consultant radiologist will probably look at the image at a later date. However, clinicians also tend to take an initial look at the exam, particularly for urgent cases, and they may not have sufficient experience to interpret the image. This is one way early findings which hold vital clues about infection may get missed," Das noted.
The 55 MERS-CoV patients fell predominantly into two categories: Of 33 admitted elderly patients who had a direct epidemiological link with a primary contact and who had a relatively higher number of associated comorbidities, 18 (55%) died due to complications and secondary infection. In the second group comprised of 22 inpatients, mainly young healthy healthcare workers, only one patient died (5%).
While patients who are young and have no comorbidities will have a better prognosis than the old and infirm, Das stressed that monitoring and quarantining patients in a hospital environment will improve outcomes and help prevent infection spread.
"If a patient from an endemic area presents with flu-like symptoms and if radiological signs such as ground-glass opacities and consolidation can be visualized on the image, clinicians should immediately perform a sputum analysis. Until it is confirmed as negative, patients should be kept at the hospital," said Das, who now works as a consultant thoracic and cardiovascular radiologist at the College of Medicine and Health Science at United Arab Emirates University in Al Ain.
To cope with the influx of patients, the King Fahad Hospital put up a temporary field hospital on the premises with multiple monitoring rooms. Outpatients suspected of infection but who were otherwise healthy or only mildly symptomatic went to the field hospital to be monitored. Outpatients who were significantly symptomatic and clearly not healthy became inpatients in the main hospital and were treated with antivirals and/or antibiotics to fight any concomitant pulmonary infections. Inpatients and outpatients with ARDS went directly to ICU for ventilator support and medication.
"The consequences of underdiagnosis are that others will get infected and patients will die. Careful monitoring using biological data and radiographic scores remains key to patient management," Das noted. "Chest x-ray is widely accessible and should be the gold standard, as images and scores chart the progression and type of disease," he concluded.
MERS-CoV was first identified in Saudi Arabia in 2012, but by June 2015 had spread to 20 other countries. In Saudi Arabia alone, there were 1,035 confirmed cases within the same period, with 458 deaths (44%), according to the kingdom's Ministry of Health. Global mortality rate approaches 60% of cases, according to 2015 statistics from the World Health Organization.