A coalition of academic organizations has released a set of appropriate use criteria (AUC) covering when multimodality imaging should be used to follow up patients with congenital heart disease (CHD). The guidelines were published online January 6 in the Journal of the American College of Cardiology.
The guidelines are designed to address the most appropriate indications for when cardiac imaging should be used in adult and pediatric patients with congenital heart disease, identifying the most appropriate imaging modalities for the evaluation and surveillance of CHD patients. The groups believe the AUC guidelines will also serve educational and quality improvement purposes to reduce the number of inappropriate imaging tests being ordered.
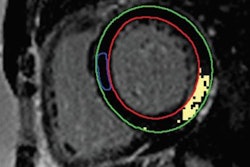
The authors note that major advances have occurred in the diagnosis and treatment of patients with congenital heart disease, but many patients are requiring long-term follow-up after cardiac surgery or catheter-based interventional procedures. Noninvasive cardiac imaging can play a major role here, with imaging tools ranging from transthoracic echocardiography to transesophageal echo, and including cardiac MRI, cardiac CT, and stress imaging.
While all of these imaging tools can be used for CHD follow-up, "there is a paucity of lesion-specific guidance for clinicians to utilize as decision-support tools," the document states. There is also much variability in the frequency with which the modalities are used, the authors wrote.
To develop the guidelines, a writing group identified the most common patient scenarios that are seen in routine clinical practice and categorized scenarios on the basis of specific cardiac lesions. Once the indications were developed, they were sent to a rating panel, which scored the use of different imaging modalities for the indication on a scale of 1 to 9, with the ratings falling into three broad categories: "rarely appropriate care," "may be appropriate care," and "appropriate care." The ratings were then subject to more discussion and debate before being finalized.
The authors noted that the scenarios in the document are based on current knowledge of patient outcomes, plus an analysis of the benefits and risks of imaging for each scenario. The authors acknowledged that clinicians will occasionally encounter patients with unique conditions that could result in the clinically indicated use of a test rated as "rarely appropriate."
"When this occurs, clinicians should document the specific situation and patient characteristics leading to this decision," the authors noted. "Thus, the AUC document should not be used as a deterrent for treating the patient or denial of reimbursement."
Development of the 47-page document was spearheaded by the American College of Cardiology, with the involvement of numerous other cardiovascular subspecialty societies. Other participating organizations include the American Heart Association, the American Society of Echocardiography, the Society for Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and others.