How can clinicians best use cardiac MRI to identify which patients with Fabry disease are most at risk for an adverse event? The mystery can be solved through two particular assessments, according to a new study published in the January issue of Radiology.
Canadian researchers found that patients with heightened left ventricular hypertrophy (LVH) and late gadolinium enhancement (LGE) are at considerably greater risk for needing an implantable device, having severe heart failure, or experiencing a cardiac death. The prognostic prowess of both parameters were further magnified as LVH and LGE levels increased.
"Identification of patients at elevated risk of adverse cardiac events is important given that cardiac involvement is the leading cause of mortality in Fabry disease and the availability of disease-specific treatment," wrote the authors, led by Dr. Kate Hanneman from the department of medical imaging at Toronto General Hospital (Radiology, January 2020, Vol. 294:1, pp. 42-49).
Fabry disease is a rare genetic condition that can adversely affect the heart by causing hypertrophy, or thickening of the heart walls. The degree of disease severity can be assessed by measuring progressive LVH, LGE, and diastolic dysfunction, which account for approximately 75% of all related deaths.
While cardiac MRI is the modality of choice to diagnose the presence of left ventricular hypertrophy and late gadolinium enhancement, existing data is limited on how well the two conditions could predict a future adverse cardiac event in patients with Fabry disease.
"Identification of imaging findings that predict adverse cardiac events is needed to enable identification of high-risk patients," Hanneman and colleagues added. "The purpose of this study was to establish the prognostic value of cardiac MRI findings in men and women with Fabry disease."
To that end, the researchers enrolled 90 patients (mean age, 44 ± 15 years), who underwent either a 1.5- (Magnetom Avanto, Siemens Healthineers) or 3.0-tesla MRI scan (Skyra Fit, Siemens) with cardiac surface coils between March 2008 and January 2019. The median time for follow-up of patients was 3.6 years (range, 2.0-6.1 years).
Subsequent adverse cardiac outcomes were defined as one of the following: rapid heart rhythm, known as ventricular tachycardia; a very slow heart rate, which required a pacemaker; severe heart failure; or cardiac death. Overall, 21 (23%) patients experienced an adverse event during follow-up for an incidence rate of 7.6% per year.
In reviewing the two characteristics, patients with LVH had a three times greater risk (hazard ratio [HR], 3.0) of adverse cardiac event compared with patients with no evidence of LVH. That risk also rose proportionally by 8% with a 5 g/m2 gain in LV mass.
Patients with LGE had a seven times higher risk (HR, 7.2) of adverse cardiac events compared with subjects with no LGE. Patients with LGE of 15% or greater were 12 times more likely to have an adverse cardiac event than patients with no LGE.
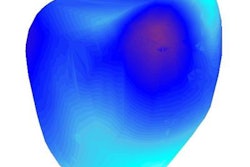
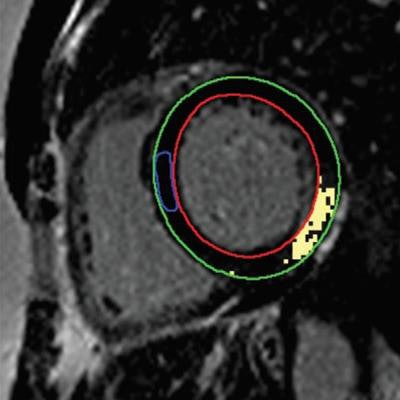
![MR images of a 45-year-old woman with Fabry disease who experienced unsustained ventricular tachycardia following cardiac MRI. Basal short-axis late gadolinium-enhanced (LGE) cardiac MRI (left) demonstrates midwall enhancement most prominent at basal inferior lateral wall (arrow). Basal short-axis LGE image demonstrates (right) quantification of LGE (epicardial contour [green], endocardial contour [red], normal reference myocardium contour [blue], and extent of LGE with signal intensity threshold of 4 standard deviations above visually normal myocardium [yellow]). Images courtesy of Radiology.](https://img.auntminnie.com/files/base/smg/all/image/2020/01/am.2020_01_06_22_36_5981_2020_01_07_Fabry_disease.png?auto=format%2Ccompress&fit=max&q=70&w=400) MR images of a 45-year-old woman with Fabry disease who experienced unsustained ventricular tachycardia following cardiac MRI. Basal short-axis late gadolinium-enhanced (LGE) cardiac MRI (left) demonstrates midwall enhancement most prominent at basal inferior lateral wall (arrow). Basal short-axis LGE image demonstrates (right) quantification of LGE (epicardial contour [green], endocardial contour [red], normal reference myocardium contour [blue], and extent of LGE with signal intensity threshold of 4 standard deviations above visually normal myocardium [yellow]). Images courtesy of Radiology.
MR images of a 45-year-old woman with Fabry disease who experienced unsustained ventricular tachycardia following cardiac MRI. Basal short-axis late gadolinium-enhanced (LGE) cardiac MRI (left) demonstrates midwall enhancement most prominent at basal inferior lateral wall (arrow). Basal short-axis LGE image demonstrates (right) quantification of LGE (epicardial contour [green], endocardial contour [red], normal reference myocardium contour [blue], and extent of LGE with signal intensity threshold of 4 standard deviations above visually normal myocardium [yellow]). Images courtesy of Radiology."These data support the necessity for future larger studies to evaluate whether cardiac MRI can be used to prospectively identify high-risk patients and to establish Fabry disease-specific prediction models," the authors concluded.