
Parents are often the first to discover retinoblastoma in their children. That's because RB's most common presentation, leukocoria, can appear in photographs as a white spot in the pupil of the eye. The past few years have yielded many clues about the childhood cancer, which occurs in about 1 in 20,000 births, is rising in incidence, and is associated with a missing tumor suppressor gene at 13q14. Yet there is scant knowledge about a particularly deadly form of the disease known as trilateral retinoblastoma (TRB), in part due to a lack of imaging studies.
At the 2001 American Roentgen Ray Society meeting in Seattle, neuroradiologist Dr. James Provenzale from Duke University in Durham, NC, discussed his team's efforts to document the progression of TRB. Specifically, the researchers sought to measure the time interval for development of leptomeningeal dissemination, and develop an imaging protocol for TRB, which occurs in about 6%-10% of bilateral RB patients, or perhaps 15-30 children in the U.S. each year.
"The term trilateral retinoblastoma refers to the presence of a midline intracranial small blue cell neoplasm in the setting of ocular retinoblastoma -- almost always bilateral ocular retinoblastoma," Provenzale said. "This midline neoplasm has variously been called a number of names, including pineal blastoma, but many current references simply call it a small blue cell neoplasm. The midline neoplasm usually occurs in the pineal region, but also can occur in other midline locations, typically in a suprasellar location, but a review of the literature shows that about 90%-95% of the lesions are in the pineal region. The tumor is very nearly uniformly fatal, with most patients dying from leptomeningeal tumor spread."
But the literature says little about the progression of TRB, where tumor dissemination is likely to occur, and whether dissemination occurs slowly or rapidly over time, Provenzale said.
"No imaging guidelines exist, so the question is, for a new patient with this entity, should solely intracranial imaging be performed? Spinal imaging? Both? And at what frequency?" he asked.
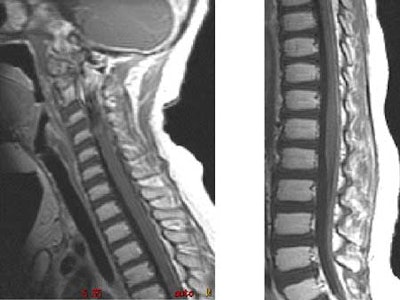
The Duke team sought to answer these questions by retrospectively reviewing the clinical records and imaging studies of 8 patients with TRB over 15 years. They looked for the presence of leptomeningeal tumor, the time of discovery of an intracranial mass, and the interval from discovery of intraspinal leptomeningeal disease. All 8 patients had cranial MR imaging, and 6 had spinal MR imaging using standard protocols.
Of the 8 patients, 6 were initially treated with chemotherapy and radiation therapy, and 2 underwent surgery and chemotherapy. One was treated initially with radiation therapy and chemotherapy, and later underwent surgery in the pineal region. All patients underwent cranial MR imaging, and 6 of 8 patients also had spinal MR imaging, Provenzale said.
Over the course of the study, six patients developed intracranial metastases as seen on MR imaging. Five of the patients developed intraspinal metastases, with four seen on MR, and one diagnosed by lumbar puncture, Provenzale said.
The time from detection of the primary intracranial mass and discovery of the intracranial leptomeningeal disease ranged from 7-26 months (mean, 13 months). Most were diagnosed within a year, however. The mean interval to discovery of intraspinal metastases was 9 months, with a range of 0-26 months.
A discernible progression pattern was seen in about half of the patients, who were diagnosed and treated for intracranial disease with some combination of chemotherapy, radiation, and surgery, Provenzale said. Following treatment, the primary intracranial tumor shrank, and there was a period of quiescence lasting from 1-4 years, followed by rapid development of intracranial and intraspinal leptomeningeal metastases.
In four patients, leptomeningeal tumor was diagnosed within 13 months of discovery of intracranial mass. Two patients have not developed leptomeningeal dissemination, Provenzale said. One patient shows no evidence of tumor dissemination after 17 months. Another remains free of leptomeningeal disease 10 years following diagnosis of the intracranial mass, "which is relatively incredible when you look at the world literature, with most patients dying within 1 to 2 years after development of TRB," he said.
 |
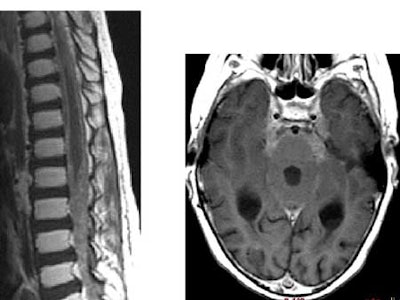 |
In conclusion, most but not all patients develop leptomeningeal tumor dissemination, he said. A quarter of the study cases have escaped it so far.
"At some point in their therapy, many of our cases had little or no residual pineal tumor at the time of discovery of intracranial or intraspinal tumor spread, so if you're looking to see where disease is going to spread in these patients, it's equally important to look at the leptomeningeal spaces as it is to look at the site of the intracranial mass, whether it be pineal or suprasellar," Provenzale said.
Finally, because spinal metastases were present in some cases at the time of discovery of an intracranial mass, Provenzale recommended that spinal imaging be performed at the time of diagnosis of the primary tumor.
"Our protocol based on this data is to perform brain and spine MR imaging at the time of diagnosis of the intracranial tumor, and then at two-month intervals in the first year, four-month intervals in the second year, and at six-month intervals thereafter.... This seems to be a very aggressive neoplasm," he said.
By Eric BarnesAuntMinnie.com staff writer
June 20, 2001
Click here to post your comments about this story. Please include the headline of the article in your message.
Copyright © 2001 AuntMinnie.com




















