Multislice CT protocol design depends mostly on scanner technology, and the rest is all about the patient, according to Dr. Mathias Prokop from the University of Utrecht in the Netherlands. At the 2003 International Symposium for Multidetector-Row CT in San Francisco, the leading MDCT author discussed strategies for maximizing protocol design.
"The main problem with computed tomography, as you all know, is that either you can improve the z-axis resolution or the scan (coverage)," Prokop said. "To a certain extent that can be altered by increasing scan duration, but it's limited to the time the patient can hold his breath."
And while conventional wisdom puts the maximum breathhold at about 30 seconds, in reality anything longer than 15 seconds is a stretch. After that "there is always a little bit of movement," he said. Fortunately, the growing number of detectors rows is making exposure a win-win situation.
"Using 16-slice CT, performance is no longer a problem, and you can optimize z-axis resolution, scan length, and scan duration at the same time," he said.
A virtual colonoscopy exam at Prokop's facility, for example, might be acquired at 16 x 0.75 collimation (table feed 8 mm/sec), covering the entire abdomen in 11 seconds. "If you add the chest, we're in the range of about 17 seconds, so it's a relatively comfortable scan considering that we're scanning with extremely high spatial resolution," he said.
Pitch
What changes in multislice CT is the definition of pitch. "There are two definitions of pitch on the market," Prokop said. "One is the definition adopted by Philips, or Marconi, or Elscint at the time. The so-called beam pitch uses the table feed divided by all of the detectors, while the slice pitch uses just a single detector width. The slice pitch (also known as volume pitch) gives you much larger numbers, which is probably the reason why most manufacturers have used it."
As for the larger question of whether high pitch or low pitch is preferable, Prokof said he generally aims high by setting the collimation first, then raising the pitch. "That means the table feed also increases," he said. "That will lead to an increased slice width, the effective slice profile gets wider, and the artifacts increase. However, if we keep our table feed, or basically scan time for the patient, constant, then in order to get high pitch we have to decrease the collimation. The resulting effect is that high pitch actually decreases the slice width, (although it) increases artifacts." Conversely, if one starts with a given table feed, raising the pitch decreases the slice width and decreases artifacts, he said.
One can easily compare the results of two imaging approaches, as long as the table feed is precisely the same for both acquisitions, he added.
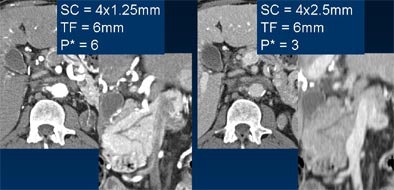 |
| Comparable image quality is seen in thick axial reconstructions of images acquired at 1.25-mm (upper left) and 2.5-mm collimation (upper right). However, coronal reformations of the pancreatic duct are markedly sharper from 4 x 1.25-mm data (lower left) compared with image acquired at 4 x 2.5 mm (lower right). SC = slice collimation, TF = table feed, P = pitch. Images courtesy of Dr. Mathias Prokop. |
On the other hand, pitch can be lowered in order to decrease artifacts, he said. This technique is especially helpful in the peripheral skeleton, in the C-spine, or in any situation where patient dose is critical, and the radiologist wants to avoid the dose spike that comes with thinner collimation.
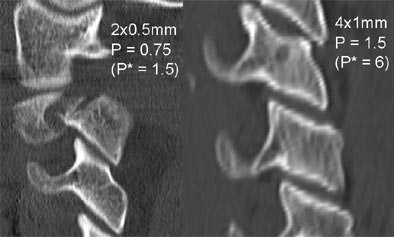 |
| Lower pitch (left) can be used to reduce artifacts in thin-section imaging, an approach that is particularly useful in the peripheral skeleton or in the C-spine, above. Images courtesy of Dr. Mathias Prokop. |
"As section collimation goes down, the four-slice scanner will see a massive increase in the CTDIvol (CT dose index volume), which means that the dose will go up by 30% for 1-mm sections, and over 200% with open 5-mm sections," Prokop said. Ultra-thin collimation should therefore be reserved for areas that can handle the increase, such as the inner ear or the peripheral skeleton, he said.
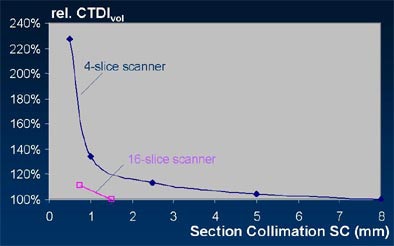 |
| The radiation dose (CTDIvol) increases dramatically with thinner collimation, although the problem diminishes as the number of detector rows increases. The thinnest collimation settings should be reserved for regions that are not dose-critical, for example the inner ear or peripheral skeleton. Chart courtesy of Dr. Mathias Prokop. |
Reconstruction and processing
Multislice scanners offer more reconstruction variables than single-slice machines, and the effective slice width depends on how the images are reconstructed, Prokop said.
The main thing to remember is to keep the slice width larger than the collimation, because if one acquires sections at 4 x 2.5 mm, for example, one cannot go back and reconstruct 1-mm thick sections. The reconstruction increment in MDCT works very similarly to that of single-slice CT: not much of an overlap is needed for viewing, but more slice overlap is necessary for MPR and 3-D imaging, Prokop said.
"As you get to thinner and thinner sections, let's say on a Toshiba scanner, to 16 x 0.5 mm, it doesn't really make sense to get a reconstruction increment (as large as) half the slice width," Prokop said. "That would give us a higher sampling rate on z-axis than the actual pixel size in our image."
Pixel size for a 350-mm cross-section is 0.7 mm, so a reconstruction interval of 0.5 mm to 0.7 mm is acceptable for most 16-slice applications, he said.
Getting the most out of multislice
Multislice users have a philosophical choice to make, Prokop said. They can approach acquisition as if they were performing single-slice CT, aiming to acquire axial slices of reasonable thickness, usually in the 5-mm range, creating multiplanar and 3-D reconstructions as needed. This approach is simple and cost-efficient, works well for nearly all imaging questions, and allows for high patient throughput.
For most applications the radiologist will want to acquire images a little thinner than in single-slice, say 4 x 2.5 mm, unless there are special questions to address, such as the presence of pulmonary embolism in high-resolution chest CT.
"But the potential of multislice CT isn't fully utilized," Prokop said. "And if you really want to do a good reconstruction it means you have to basically keep your raw data until you or your fellow radiologists have seen the images, and see if they really need high resolution."
The volumetric reconstruction approach that Prokop and colleagues use changes both reading considerations and workflow. The group relies on thin-slice acquisition to produce a secondary, nearly isotropic dataset that actually looks quite poor unless MPRs or 3-D reconstructions are created from it, if needed. The need to store and process the secondary dataset makes this approach more expensive and time-consuming than traditional methods, but it does make full use of MDCT's capabilities, he said.
Prokop's group counters the productivity shortcomings of the isotropic approach with real-time interactive viewing of the dataset. More vendors are beginning to offer this capability, and the quality of the results is very high, he said.
"Our scanner allows us to interactively adjust the thickness of the slice just so that the signal-to-noise (ratio) is just as you like it, and go through the axial sections, and the coronal, and maybe the sagittal. It takes about the same time it took to read the conventional single-slice scan, but you have all the multiplanar information available."
Even with minimal radiation dose, diagnostic images can be obtained by acquiring a near-isotropic secondary dataset and reconstructing with thicker slices in any plane.
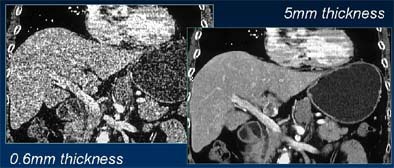 |
| Reconstructing thicker sections (at right) reduces noise in low-dose, thin-collimation image acquisition. Images courtesy of Dr. Mathias Prokop. |
A good way to begin maximizing MDCT's capabilities is to perform real-time interactive viewing of isotropic 3-D volumes using 16-slice data. The approach can even be used with four-slice scanners once radiologists get used to it, Prokop said, adding that to do so, four-slice scanners will generally have to acquire images in fast spiral mode.
Of course, isotropic datasets, with anywhere from 0.5 to 2.5 GB of data per exam, add up to about 5 terabytes annually at 10,000 exams per year. This may sound like a lot of data, but the free-market cost of storage is less than $2,000 per terabyte, he said. Vendors charge much more per terabyte, of course, but the long-term cost of storage continues to drop, making the isotropic approach a reasonable one.
"When we're doing image review on the workstation, we're looking (only) at thick sections, and reconstructing thick axial sections and MPRs on the fly," he said. "We reconstruct thick axial sections for our clinicians so that they still have conventional CT scans, and these will be accessible to them on the PACS."
The alternative is to provide interim storage of the isotropic datasets for up to three months. That way, follow-up diagnostic questions can be answered with thin-section reconstructions, without the need to store large quantities of data permanently.
Dose discussion
Designing protocols also means creating low-dose techniques for children, and for imaging benign disease such as PE, pancreatitis, ureter stones, or inflammatory bowel disease, as well as all screening examinations, Prokop said.
"Very frequently you don't have to do a four-phase liver or four-phase kidney stone (exam)," he said. "Sometimes you have to ask yourself which diagnostic questions will let you drop which of these phases. If you do that, the dose goes down substantially."
The thicker the MPR slices, the lower the dose can be, he said. The automated exposure controls now available from most vendors allow a significant reduction in dose, and enable the CTDIvol to be adapted for each patient.
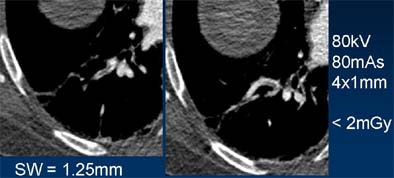 |
| Low-dose CT reveals even very small pulmonary emboli. Images courtesy of Dr. Mathias Prokop. |
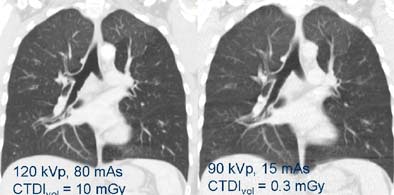 |
| Even extremely low-dose imaging can often answer the relevant clinical questions, especially in high-contrast areas such as the lungs. Image at right was acquired with 1/30th the dose of example at left; both reveal air trapping. Images courtesy of Dr. Mathias Prokop. |
"In summary, the general rule we have is to use thin collimation and high pitch, with the exceptions that I mentioned," Prokop said. "Use a thin secondary dataset and reconstruct thick axial sections or MPRs for review. With 16-slice CT, speed is no longer an issue. Five to 10 seconds is the usual scan time for chest and abdomen, and volume imaging becomes the standard. One- or 2-mm slice widths for most applications can easily be done, and thick multiplanar reconstructions should be done. I think the worst case is to become a traitor to (MDCT's capabilities) in designing your protocols."
By Eric BarnesAuntMinnie.com staff writer
August 22, 2003
Related Reading
Ask questions to optimize MDCT protocols, July 11, 2003
Pediatric CT won't stop growing, but dose can be minimized, May 8, 2003
Copyright © 2003 AuntMinnie.com