Mention soccer injuries and most people think below the belt -- injuries sustained in the lower extremities while trying to bend it like (David) Beckham, pull off a Mia Hamm-style fake-out goal, or simply keep up with 14-year-old wunderkind Freddie Adu.
But heading the ball is a significant part of the soccer player's arsenal, and, as a result, players must also contend with cervical spine trauma.
Reports out of Japan and Norway found that players who regularly headed the ball over their career had a higher incidence of cervical spine degeneration. Radiographs revealed abnormalities including calcification of the anterior longitudinal ligament, anterior and posterior vertebral spurs, and ossicles on or between spinous processes (Sports Medicine, September 1992, Vol. 14:3, pp. 200-213; Skeletal Radiology, 1991, Vol. 20:6, pp. 437-440).
More recent research reiterated those findings. A group from Cankaya University in Ankara, Turkey, looked at the early onset of cervical spine degeneration in 30 active and retired soccer players. They used x-ray and MRI to evaluate dynamic changes in the spine.
"Degenerative changes were prominent in veteran players ... 10-20 years earlier than that of the normal population. Magnetic resonance findings of the degeneration were more prominent in soccer players ... most probably due to the high- and/or low-impact recurrent trauma to the cervical spine caused by heading the ball," they wrote (European Spine Journal, February 2004, Vol. 13:1, pp. 76-82).
When it comes to diagnosing and following patients with cervical spine trauma, multidetector-row CT (MDCT) is rapidly becoming the modality of choice, according to a presentation at the 2004 International Symposium on Multidetector-Row CT in San Francisco by Dr. Jay Cinnamon of Quantum Radiology Northwest in Marietta, GA.
Cinnamon offered a brief historical overview and a breakdown of the technological advances that may make MDCT the ideal imaging modality in cervical spine trauma.
"We know that CT can confirm fractures suspected on plain films. CT can also better characterize the fracture and detect additional fractures," Cinnamon said.
"CT can rule out fractures more effectively. So if you have plain films that are equivocal, CT can come in and kind of save the day." Plus, he noted, "CT can provide some info about the soft tissues, such as a traumatic herniated disk or an epidural hematoma."
Newer capabilities
The limitations of conventional CT studies prior to spiral imaging included the length of the study and an inability to identify certain types of fractures, such as facet, pedicle, laminar, and in-plane vertebral body fractures.
According to Cinnamon, these fractures essentially fall into two main categories. They are either very small, bony fragments such as laminar fractures, or in-plane of the CT section fractures. The latter may be difficult to detect using 3-mm slices, he said.
So what should radiologists look for when they do a CT scan of cervical spine trauma? Osseous findings include the extent of the primary fractures, any associated fractures, and evidence of instability, such as perched or subluxed facets.
"You want to look for retropulsion of bone and compromise of the spinal canal," Cinnamon said. "You want to look for subluxation. These are the bones that you are going to focus on when you do your CT study,"
"Especially if you have a patient with jumped facets, you want to be looking for traumatic disk herniation," he added. "Before the surgeons reduce that jumped facet and subluxation, they want to know if there is a disk herniation. If there is, reducing the cervical spine can make things a lot worse."
CT has advanced and now offers information that x-rays cannot begin to provide, he noted, citing the case shown below (images A-E).
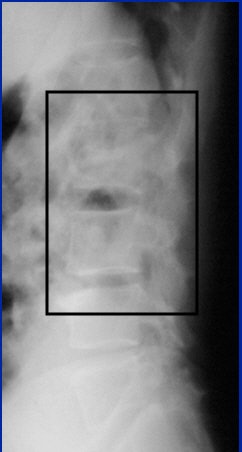 |
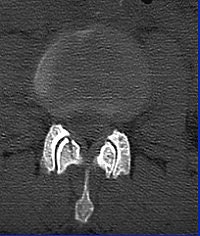
Image A
 |
"Here the patient has an L-2 fracture that you can see. Notice the quality of the image isn't very good. That's important because in the trauma setting, you can't always get good-quality images. You can make the diagnosis of an L-2 fracture on the plain films, but you can't characterize it until you get to CT," Cinnamon explained.
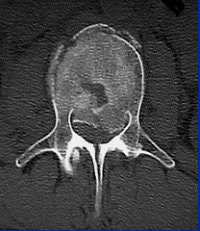 |
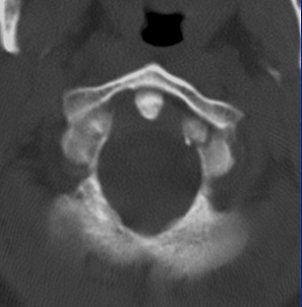
Image C
  |
"With CT, you see that it's not just a compression fracture of the superior endplate, but really it's a burst fracture involving the anterior, middle, and posterior columns. The fracture goes through the vertebral body (with) retropulsion of bone, and it goes through the spinous process, through the lamina, and even into the facet joint."
Soccer spines
Fractures are certainly a risk factor for soccer players. Cervical injury accounted for 83.5% of all spinal cord injuries in soccer players, as well as divers, rugby, and football players, according to a Japanese study. Fractures can occur from contact between players, or between a player and the ball (Spinal Cord, July 1996, Vol. 34:7, pp. 416-421).
"In the case of soccer, it is wise to avoid using older (worn) equipment. Soccer balls are made of leather, and can therefore absorb up to 20% of their weight in water," according to the DynoMed.com patient encyclopedia.
In fact, a wet ball contributed to one case study. In this instance, a 16-year-old athlete developed pain after being dropped on his head with a flexed neck while wrestling with his younger brother. The patient was diagnosed with neck and shoulder strain, but he continued to experience pain in his neck and arm -- a pain that worsened after he headed a wet soccer ball.
Plain radiographic studies were all read as negative by an emergency room physician. With his persistent symptoms, doctors then turned to CT, which showed a nondisplaced linear fracture of vertebral body C-7 (The Physician and Sportsmedicine online, December 1997, Vol. 25:12).
"Most sports-related fractures and dislocations of the cervical spine occur in the lower cervical segment, C-4 to C-7, and most severe injuries involve fractures of the vertebral body with varying degrees of compression or comminution," explained case study author Dr. Rocky Khosla, director of sports medicine for the Southern Colorado Family Medicine Residency Program in Pueblo.
"These injuries usually occur with axial loading of the neck in flexion; when the vertebral column loses its normal curve, the axial force is transmitted down the straightened cervical column," Khosla added.
Although a six-month follow-up CT showed the parasagittal fracture had nearly healed, the patient was advised to avoid contact or collision sports indefinitely.
In many cases, these fractures occur because the cervical spine is already compromised by a degenerative condition such as disk disease, spondylosis, and stenosis. Athletes who participate in collision sports are also reportedly more susceptible to functional stenosis (Techniques in Surgery, June 1999, Vol. 5:2, pp. 185-193).
"Functional stenosis exists if the protective cushion of surrounding cerebrospinal fluid around the cervical cord is obliterated," wrote Drs. Mark Giovanini and Arthur Day from the department of neurosurgery at the University of Florida in Gainesville.
The neurosurgeons recommended that athletes with suspected cervical stenosis undergo a battery of imaging tests -- x-rays, CT myelography, MRI, dynamic flexion-extension studies -- to rule out irreversible neurological consequences. These test results play a major part in determining whether a player can go back to the pitch.
Strategies for CT
In his presentation at the MDCT meeting, Cinnamon proposed five potential strategies for CT imaging of the cervical spine. The first is the most conservative: stick with x-ray and only use CT as a secondary tool if necessary. Another option is to set a low threshold for CT. For example, a patient with questionable findings on x-ray automatically goes on for a CT scan. The third is a model of convenience. For example, if a patient is getting a head CT, then it may be convenient to do a cervical spine CT as well, he said.
"The fourth model is CT for everyone," he explained. "You got hit in the head with a golf ball? You just bought yourself a CT of the spine."
Finally, there are stratified risk groups whereby patients selectively undergo CT based on the initial clinical evaluation. But, Cinnamon warned, "This requires some thinking and ... lots of guts on the part of clinicians to not give in to the pressure of the medical-legal environment."
Whichever model is chosen, Cinnamon advised paying attention to the inverse relationship of contrast and spatial resolution, using the following case as an example (images F-G).
 |
| Image F |
"On the 2.5-mm slice, you can see the occipital condyle fracture. If (you) go down to the 0.5-mm slice, you can see the fracture just as well -- maybe it looks a little sharper. But you can still identify the fracture on the thicker slice. The value for this is on the coronal and sagittal reformatted images from the 2.5-mm axials. There's a tremendous amount of stair-step artifacts. On the 0.5-mm images, you've eliminated the stair-step artifact because your spatial resolution is so good."
 |
| Image G |
Cinnamon urged his fellow radiologists to consider offering 3D images to the surgeons. Surgeons often don't ask for 3D images, which can be very helpful for visualizing the fracture and treatment planning, he said.
 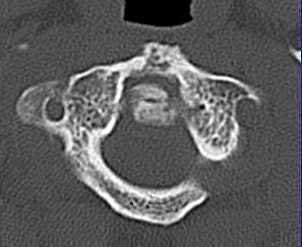 |
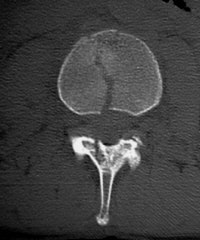
The 0.5-mm slices offer fine bone detail, but pay a price on the soft-tissue images in terms of soft-tissue differentiation. Whereas the thicker (5-mm) slices fail to show the bone detail of the fracture well, but possess greater contrast resolution on the soft-tissue window to differentiate spinal cord from surrounding spinal fluid.
  |
One caveat for cervical CT pertained to clearing the C-spine. If ruling out instability is the goal, it is important to start with a static radiological evaluation to look for fractures, Cinnamon said. Dynamic radiological evaluations, such as a flexion-extension exam or dynamic MRI, may also be necessary because CT alone cannot evaluate for instability.
Paradigm shift?
If the plan is to go with CT all the time with the cervical spine, Cinnamon urged his audience to break free of traditional imaging protocols.
"You have three axes along this patient's (lumbar) spine: The anteroposterior axis, the lateral axis, and the longitudinal axis. Which is the longer axis? The longitudinal axis. The more conventional way we've always looked at this is with a whole series of axial images. Why should you do that? Instead of looking at the spine in the axial (plane) -- and using the reformatted images as bells and whistles to tell you whether there is subluxation -- why don't you use the coronal and sagittal reformatted images as the primary diagnostic tool? They are going to be every bit as good as the axials," he said.
"If we are going to embrace multislice CT, don't think of it as slices anymore," Cinnamon added. "Think of it as volumetric, isotropic data -- pure, robust data. That robust data can be portrayed in multiple different ways."
By Shalmali Pal
AuntMinnie.com staff writer
August 18, 2004
All images courtesy of Dr. Jay Cinnamon.
Related Reading
Heading balls may damage footballers' necks, February 19, 2004
Boning up on musculoskeletal MR basics at ISS, September 18, 2003
The lowdown on lumbar spine positioning, June 19, 2003
CT-guided spinal intervention alleviates low back pain, May 6, 2003
Radiographic positioning techniques for the cervical spine, March 26, 2003
Plain film x-rays not needed with CT to evaluate polytrauma spinal injuries, December 6, 2002
Copyright © 2004 AuntMinnie.com




















