
Even when an experience is less than optimal, it can still be a great teacher. In the case of a recent multicenter VC trial that yielded disappointing results, radiologists took the time to learn where, how, and why lesions were missed.
The just-published multicenter trial compared colonoscopy to VC to air contrast barium enema (ACBE) in 614 patients with a positive fecal occult blood test. VC's per-patient sensitivity for lesions 10 mm and larger (n = 63) was 59% (46-71, p = 0.1083 for VC versus ACBE), compared to 48% for ACBE (95% CI 35-61), and 98% for colonoscopy (91-100, p < 0.0001 for colonoscopy versus VC). Specificity was 99% for colonoscopy, 96% for VC, and 90% for ACBE for lesions 10 mm and larger, declining for VC when smaller lesions were considered. And for lesions measuring 6-9 mm, sensitivity was 35% for ACBE, 51% for VC, and 100% for conventional colonoscopy (The Lancet, January 15, 2005, Vol. 365:9455).
Considering that the study was designed in 2001, researchers from the Duke University Medical Center in Durham, NC, chose a respectable technique for their VC exams: CT was performed with a four-slice scanner or better, using 2.5-mm collimation and 1-mm reconstruction intervals. Prospective 2D reads with 3D problem solving was used for interpretation on Vitrea 2 software (Vital Images, Plymouth, MN).
Yet the protocol lacked some of the bells, whistles, and, well, refinements seen in more recent exams -- such as CAD overreads, stool and fluid tagging, electronic subtraction of fecal material, and the like. Some readers were relatively inexperienced. And the challenging, symptomatic FOBT-positive cohort itself might have complicated interpretation. But the trial offered an excellent opportunity to examine the unaided VC exam, and identify areas for improvement.
In a presentation at the 2004 RSNA meeting in Chicago, Dr. Erik Paulson, chief of abdominal radiology at Duke and lead radiologist in the study, re-examined a subset of the results to determine which lesions had been missed prospectively and why.
"The purpose of this (second) paper was to retrospectively review missed lesions on CTC (VC) using a subset of patients from a recently completed multicenter prospective trial, (aiming) to understand the cause of the miss, and determine if the miss was technical or perceptual in nature," Paulson said in his December talk.
In all, the retrospective study looked at CT images from 288/614 prospective trial participants, all of whom had been examined at the Boston and Durham, NC, sites in which Paulson was a participating radiologist.
Two readers, one experienced in VC and one not, reviewed 32 cases representing lesions missed on VC but found on conventional colonoscopy from the two sites. The workstation was loaded with the same Vitrea 2 software used in the original study. And the reviewers knew the size, location, and morphology of the missed polyps before they began.
Of the 32 total missed lesions, 23 were adenomas, one was a cancer, and six were hyperplastic polyps. Thirteen of 32 were considered errors of perception, 15 were technical errors, and four were not yet reviewed, Paulson said.
"Those things that you could identify retrospectively we identified as misses, those were perception errors," he said. "In those cases where we could not find the polyp (retrospectively on CT) despite our best efforts, we considered those to be technical errors, and we looked for contributing factors."
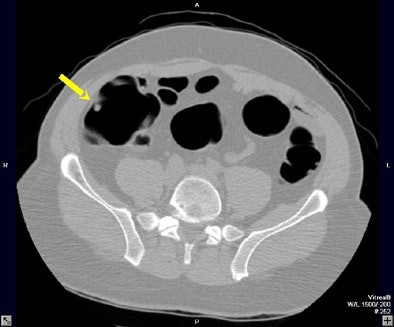 |
| A 6- to 9-mm adenoma in the ascending colon was missed due to perceptual error. Above supine axial image through the ascending colon. The arrow points to a 6- to 9-mm polyp, which was not seen on the initial interpretation. Below, 3D endoluminal view shows the polyp (arrow) on a fold. Images courtesy of Dr. Eric Paulson. |
 |
Ten of the 13 perceptual errors were "flat-out misses" in which the lesion could be seen in retrospect, Paulson said. Eight of the 13 were polyps located on a haustral fold. In nine of the 13, the polyp could be seen on one view -- prone or supine -- but not the other view, due to residual fluid or a collapsed bowel segment. And there were two missed sigmoid adenomas in the setting of impressive sigmoid diverticulosis that may have contributed to the misses, he said.
The one missed cancer, in the cecum, was a challenging perceptual error, he said. Nothing unusual was seen on the ileocecal valve prospectively; even retrospectively its appearance was only slightly thickened, but "on the sagittal reformation is a retrospectively seen shelf and that shelf proved to be a 30-mm adenocarcinoma," Paulson said.
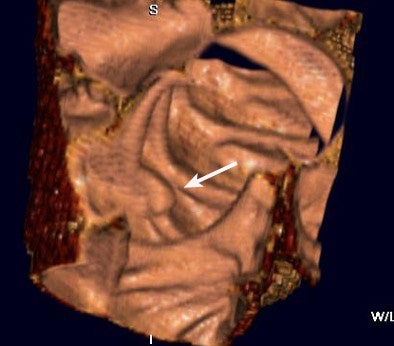
There were 15 technical errors, and in seven of the 15 the lesion could not be identified retrospectively despite excellent bowel prep and good distension. Of these, he said, four were flat lesions, and three were located on a fold. Other technically challenging cases were complicated by the presence of stool or fluid in the involved segment, or by failure to achieve good distension in the involved segment. A breathing artifact prevented visualization of an 8-mm polyp in one patient.
 |
| A colonoscopically and pathologically proven 6- to 9-mm polyp in the transverse colon cannot be seen, even in retrospect, due to technical error. Above, representative axial image shows excellent preparation and distension of the transverse colon. On both the prospective and retrospective interpretation, no lesion could be identified in the transverse colon. Below, coronal reformation of the transverse colon shows good distension and good preparation. There is some motion artifact (arrows) from breathing which minimally obscures a portion of the transverse colon. |
 |
The location of missed lesions was mainly right-sided, including two in the cecum, 10 in the ascending colon, 11 in the transverse colon, two in the descending colon, six in the sigmoid, and one in the rectum, Paulson said.
Both technical and perceptual errors account for misses on virtual colonoscopy, Paulson concluded, adding that others have seen similar results in studies that used 2D with 3D problem solving, and no stool tagging or electronic subtraction.
"How could we do better? I think stool and fluid tagging may play an important role, and perhaps would have increased our sensitivity," Paulson said. "Perhaps the fly-through technique would have increased our detection rate, or fly-through combined with subtraction or CAD will likely prove useful. And finally, a compulsive reading technique is critical in looking for polyps."
By Eric Barnes
AuntMinnie.com staff writer
January 17, 2004
Related Reading
Colonoscopy still best for detecting colon cancer, December 20, 2004
Duke VC trial results disappointing, November 1, 2004
Gastroenterology warning: Prepare for VC or regret it, October 6, 2004
VC faces off (again) against second-look colonoscopy, October 4, 2004
VC fares better as its own gold standard, September 8, 2004
Copyright © 2005 AuntMinnie.com




















