In our second and final installment of AuntMinnie.com's series on CAD, we take a look at issues such as reimbursement, workflow, and the technology's burgeoning role in multislice CT and virtual colonoscopy.
In general, reimbursement is the ultimate determining factor in the success of new imaging technologies. But for some institutions, reimbursement for CAD isn't a priority.
"Breast MR -- and MR, in general -- is expensive enough. We don't layer on additional costs," said Andrew Osiason, director of abdominal imaging for New Century Imaging in Oradell, NJ. For the quality of work they're trying to achieve, CAD is a necessary part of the practice and they don't want to pass the costs on to the patients to incur additional charges, Osiason stated.
Dr. David Mendelson, an associate professor of radiology at the Mount Sinai School of Medicine in New York City, is a chest radiologist who has been working with R2 Technology's CAD product for chest CT for about a year. Although lung CAD is not reimbursed, he offered a similar view.
"I believe that a second read -- while it may not be regarded as mandatory -- is very beneficial to the service you are delivering to your patient," he said. "I would hope that just as breast CAD is reimbursed, we reach a point where lung CAD is reimbursed."
As for workflow, Mendelson uses CAD to read, on average, two lung cases per day, though the technology can easily handle a greater volume. Images are sent for R2 CAD review from the CT scanner and the facility's PACS.
"Once there, you give it five minutes to process and there is a summary report," Mendelson said. "The technology makes it very easy for missed nodules to appear with one click."
While CAD doesn't shorten Mendelson's day, it does prompt him to review missed, potentially cancerous lung nodules. It takes literally two seconds, he said, to recognize a false positive or a nodule that requires additional review.
 |
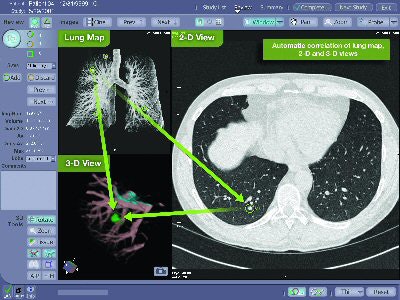
| Lung map (upper left corner) depicts CAD-detected nodules, which are then indicated by a green circle in the 2D axial view. An automatically generated 3D volume rendering (lower left corner) can be rotated in real-time to further analyze the finding. Image courtesy of R2 Technology. |
CAD also helps radiologists in dealing with multiple CT images, though it doesn't assume all the responsibility.
"I still have to look at the image," Mendelson said. "It is a quality issue, the human failure rate. If you have to look at 300 images, you are probably more likely to miss something, quite frankly. That's what we are hopefully eliminating with (CAD) as a backup."
Multislice CT
Dr. Mary Roddie, consultant radiologist at Charing Cross Hospital in London and advisor to CAD firm Medicsight, also of London, estimates that she views 1,400 to 1,600 images when reading general multislice CT and colonography scans. Medicsight has proposed that its Colon CAR (computer-assisted reader) be used as a joint reader, so potential polyps are displayed on first review, rather than making a radiologist return to look a second time, thus prolonging the process.
"I think radiologists are very good at taking in a lot of information very quickly. What we are not good at is the boring, repetitive looking at every little fold in the colon to see if there is a polyp there," Roddie said. "How we implement (CAD) into the workflow will be critical. I suspect that the concept of the joint read will be the most effective way of implementing that into practice."
Roddie uses Medicsight CAR technology in her clinical practice for CT colonography and thoracic CT examinations to screen for nodules. The software has been effective in detecting lung nodules of 2-3 mm in size, she said, though she tends not to act on them unless the nodule is 5 mm or larger.
"My consideration is that anything smaller than (5 mm) will not be significant," Roddie said.
The results, however, do provide a baseline scan so the 2- and 3-mm nodules can be monitored to see if they enlarge and how quickly, Roddie said.
 |
| Click here to enlarge this image. |
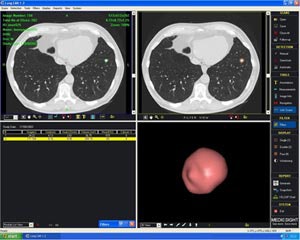
| Polyp enhancement filter (PEF) acts as a joint or concurrent reader with the radiologist turning off the filter to evaluate any potential polyp candidate highlighted by the filter, according to Medicsight. Image courtesy of Medicsight. |
The issue of true or false positives in detecting nodules or polyps is more serious in lung cases, given the more extensive follow-up involved. In the case of a lung nodule, a needle biopsy or surgery may be the strategy, consequences that Roddie says are relatively more serious than a colonoscopy if it turns out that a patient didn't need any follow-up procedure. Again, here is where CAD can be a valuable tool.
"I don't think CAD will show me something that I would falsely call a nodule," Roddie said. "I am much more worried about missing a nodule."
False positives
The University Health Network of Toronto has commenced a study to evaluate CT CAD technology in lung cancer screening, an initiative overseen by Dr. Heidi Roberts, a radiologist and associate professor of radiology in the university's department of medical imaging. The study currently is analyzing some 250 lung cases, retrospectively validating the CAD results using products from R2 Technology's ImageChecker CT and Medicsight's Lung CAR systems.
Though it is too soon to calculate a false-positive frequency in the study, Roberts described false positives detected by the two companies' technologies so far as "easily dismissible," noting that "there are hardly any false positives that require extensive workup." Nodule detection has ranged in size from 1-15 mm, she said.
Roberts is in line with colleagues who say that CAD will never replace a radiologist, adding that the potential for CAD is as a second reader.
"(CAD) does improve the performance of radiology," she said. "It tends to find nodules that were missed by the reader, and it finds different nodules in different areas that might have been overlooked."
Workflow issues
If CAD is having a positive impact on workflow, then something in the department is amiss, according to one radiologist.
"CAD should virtually never improve your workflow if used according to manufacturers' or researchers' recommendations," said Dr. Jay Baker, chief of the breast imaging division at Duke University Medical Center in Durham, NC. "If it improves workflow, it implies that you were not doing something before and you are letting CAD do it instead."
Duke has used R2's ImageChecker for the past three years to screen all of its film-based mammograms.
"It takes two to four minutes to digitize each case," Baker said. "So, we have reviewers in the diagnostic reading room ready to be used, while the technologist essentially is waiting for the films to come out of the digitizer, or someone would have to pick up the films and bring them to us."
Duke currently is installing its first full-field digital mammography (FFDM) system, but Baker does not expect to add CAD because of the expense to do so. Duke's radiologists batch-read about 50 mammography cases per day, with the standard allotment of four images per case.
"We read the studies the same as before, looking just as carefully for masses, distortions, and calcifications," Baker says. "We're using CAD as the backup. Frankly, it can only slow you down, because it makes you go back and look at images that you may have blown by the first time. I am not saying that is a bad thing, but it should not improve workflow."
CAD and VC
CAD's deployment in CT colonography is seen as one of the next major advances needed to foster virtual colonoscopy, according to Dr. Abraham H. Dachman, a professor of radiology at the University of Chicago in Illinois.
Dachman is a strong advocate of CAD utilization as a second read, that every patient should be evaluated in both 2D and 3D views, and that virtual colonoscopy should be in the domain of the radiologist.
"CAD has not yet solved the problem of flat lesions," he said. "It doesn't mean that CAD can't do flat lesions, but no one has developed that yet. Flat lesions are important; therefore, I believe every patient, to some measure, should have a primary 2D read and a 3D read."
Dachman collaborated on the development of CAD and virtual colonoscopy with Dr. Hiro Yoshida, an associate professor of radiology at Harvard Medical School in Cambridge, MA, when Yoshida was in Chicago. Given the number of slices generated by multidetector CT scanners, CAD's help is warranted, Yoshida said. CAD virtual colonoscopy has the potential to achieve "reasonably high performance" with high sensitivity and relatively low false positives, he added.
"The computer can reach about 90% to 95% sensitivity with about two false positives per scan, and 80% to 90% sensitivity in detection of polyps larger than 6 mm," Yoshida said. "Over 90% sensitivity is satisfactory if it is consistent. If a computer can achieve a sensitivity of more than 90%, I think it is hitting its plateau."
By Wayne Forrest
AuntMinnie.com contributing writer
July 15, 2005
Click here for "Part I: Computer-aided detection marking new targets."
Related Reading
VC CAD shows progress toward clinical use, June 3, 2005
CAD struggles through tagged, subtracted VC data, May 18, 2005
Support vector machines boost accuracy of VC CAD, May 3, 2005
CAD segmentation for mammo acceptable -- except in heterogeneously dense breasts, April 26, 2005
CAD offers promising second opinion, even in dense breasts, March 15, 2005
Copyright © 2005 AuntMinnie.com




















