Radiation doses for chest CT vary substantially depending on the application, the scanner parameters, patient particulars such as gender, and the use of automated dose modulation. But whether the baseline scan radiation dose is 3 or 6 mSv, adding retrospective electrocardiographic (ECG) gating can easily double it.
The patient-management question is whether the diagnostic value of ECG-gated pulmonary images justifies the higher radiation burden. And the answer is that it does, sometimes, according to Dr. Joseph Schoepf, associate professor of radiology and director of CT research at the Medical University of South Carolina in Charleston.
"We performed a study that was published in Radiology (December 2004, Vol. 233:3, pp. 927-933) last year, and we found that pretty much every vascular structure in the thorax does benefit from ECG gating," Schoepf said.
The benefits of crystal-clear gated images are particularly noticeable when reconstructing images from late diastole, Schoepf said in a talk at the 2005 International Symposium for Multidetector-Row CT in San Francisco.
But pretty images do not a diagnosis make. And one structure that never needs gating for diagnosis is the descending aorta, he said. "Whatever you do with (the descending aorta), it has excellent image quality and can be easily evaluated. So you don't really need to gate it ... if you know (that's) where the problem is."
Occasionally in lung parenchyma
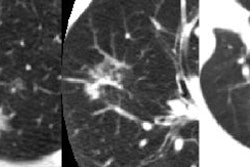
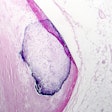
Lung parenchyma evaluations, on the other hand, sometimes benefit from gating, which can erase a number of colorfully named but pesky phenomena such as the "tram-track" artifact, the "twinkling star" artifact, and the double contours of the cardiac borders, all of which can prevent a correct diagnosis in certain circumstances.
 |
| Tram-track and double cardiac contour artifacts. Non-ECG-gated thin-section CT scans obtained at the same level of the paracardiac parenchyma in a 25-year-old man with spontaneous pneumothorax. Note the double contour artifact seen in the blurred cardiac border (arrow). Tram-track artifacts can be seen in both the right and left interlobar fissures (arrowheads) (Radiology, 1999;212:649-654). |
In a 1999 study, Schoepf and colleagues from the University of Munich in Germany aimed to identify the benefits of prospective ECG triggering for examining the lung parenchyma using high-resolution CT (Radiology, September 1999, Vol. 212:3, pp. 649-654).
"You can see that ECG triggering takes care of those twinkling star artifacts adjacent to the left cardiac border," he said of an image projected on the screen. "You get rid of what has been dubbed the tram-track sign, the double appearance of the (lung) fissures, and the double cardiac border."
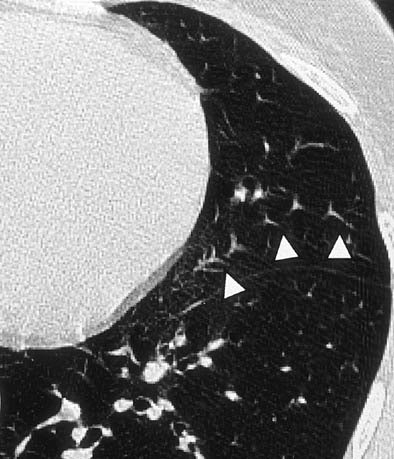 |
| Twinkling star artifact. Non-ECG-gated CT scan in a 35-year-old woman with recurrent pneumothoraces reveals "twinkling star" artifact (arrowheads). A motion artifact caused by distortion of pulmonary vessels due to cardiac motion is seen in the lingula of the left upper lobe (Radiology, 1999;212:649-654). |
Still, the study concluded that improvements in diagnostic information usually do not justify the increased radiation dose.
Rarely when imaging nodules
Pulmonary nodules are even trickier, Schoepf said. A group from the University of Ulm in Germany recently reported that prospectively gated contrast-enhanced CT images acquired sequentially detected a total of 26% more pulmonary nodules than unenhanced CT on a four-detector scanner.
For tumors smaller than 5 mm, the detection rate was 62% higher using ECG-triggered scans (p = 0.024), the group wrote. Mediastinal structures in particular were better visualized using gated CT (Academic Radiology, May 2005, Vol. 12:5, pp. 614-619).
However, Schoepf cautioned that the benefit of seeing more nodules could be outweighed by the risk of actually missing nodules due to the use of sequential imaging.
"In my experience, it's probably not worthwhile doing (gating) for pulmonary nodules in general," he said. "I think we need more data to determine if there is any benefit in nodule detection and characterization, and I would argue that there is not."
In lung parenchyma imaging, the improvement in diagnostic information resulting from gating is rarely enough to justify the added radiation dose, especially when the protocol is limited to retrospective gating, as his group's is, Schoepf said.
Sometimes for pulmonary arteries
Pulmonary artery imaging is another matter. When needed to answer a specific diagnostic question, gating can provide far cleaner delineation of the arterial branches, especially of very small branches in the vicinity of the rapidly beating left ventricle, Schoepf said.
"We looked at that in a little bit more detail from the same study published last year (Radiology, 2004), where we showed that image reconstruction can decrease those stairstep artifacts that mar evaluation of the pulmonary artery tree," Schoepf said. Gating also eliminated stairstep artifacts, vessel double contours, and artefactual hyperattenuation, he said.
At his facility, a scan to determine status after a lung transplantation in a young man posed a real diagnostic problem because the radiologists couldn't see the vessels adjacent to the heart, and there appeared to be areas of hyperattenuation in those vessels on the ungated scan, Schoepf recalled.
"We repeated the scan with ECG gating and found there was no pulmonary embolism -- obviously in that patient scenario there were critical decisions hinging on the diagnosis of pulmonary embolism," he said. "And that's how we use the (gated) test. These days we use it as a tiebreaker in those equivocal cases when therapeutic decisions hinge on the presence or absence of PE in those vessels."
Do gate the ascending aorta
"The structure you always want to gate is the ascending aorta," Schoepf said, detailing the regrettable case of a 31-year-old woman who presented to the emergency department with acute chest pain.
Reading her ungated CT scan, an upper-level resident on night call mistook a double contour artifact for a dissection flap in the aortic root, noting for good measure a slight thickening in the descending aorta. But when the patient was taken to surgery and her chest opened, the surgeons found only mediastinitis -- certainly no indication for surgery.
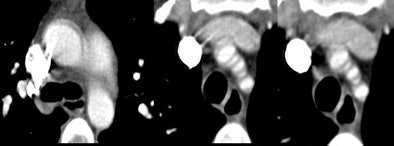 |
| A 31-year-old woman presenting with acute chest pain underwent needless chest surgery when a double contour of the aortic root was mistaken for a dissection flap. Image courtesy of Dr. Joseph Schoepf. |
Never mind that a more experienced observer might have avoided such a pitfall, Schoepf said. "You want to avoid that at all costs -- and ECG gating is a good means of doing that."
Gating also enables the diagnosis of cardiac involvement in dissection, such as continuation of a dissection into the coronary arteries, he said.
"Retrospective ECG gating should be used mainly for two applications in the chest: for the pulmonary arteries and as a problem-solving tool," when critical therapeutic decisions are being made, Schoepf concluded.
"Always gate the ascending aorta for suspected injury, rupture, or dissection .... simply because your chance of (misdiagnosis) is much decreased, to the benefit of your patient," he said.
By Eric Barnes
AuntMinnie.com staff writer
August 29, 2005
Related Reading
Scores of detector rows bring opportunities, challenges to CT imaging, April 8, 2005
ECG-gated MDCT enables accurate assessment of pulmonary nodules, November 24, 2004
Study documents rising use of CT for suspected PE, October 11, 2004
Electrocardiographic gating reduces cardiac motion artifacts in CT of the lung, September 1, 1999
Copyright © 2005 AuntMinnie.com