A decade into the game, lung CAD appears to work well enough to be considered a serious tool for screening CT lung data. Several studies have shown gains in detecting clinically significant nodules.
So why don't more radiologists use CAD in daily practice? There are many reasons, most revolving around workflow and practice issues rather than the efficacy of CAD itself, according to a talk at Stanford University's International Symposium on Multidetector-Row CT in San Francisco.
In his presentation, Dr. Jeffrey Mendel, chairman of diagnostic radiology at St. Elizabeth's Medical Center in Boston, was clear about why lung CAD is useful.
"When people say 'Why CAD?' I say 'Where's Waldo?'" Mendel said of the elusive children's book character he'd flashed on the screen. Unfortunately, radiologists also miss Waldo, or rather pulmonary nodules, all the time. "There are many articles out there showing how we fail to find pulmonary nodules in 20% to 30% cases -- and we need to have a tool to aid us in doing that," Mendel said.
CAD could help wade through the data deluge as well. Multidetector-row CT (MDCT) has ushered in exponential growth in the number of thin-section lung images radiologists have to read, resulting in more thin slices and more detected nodules.
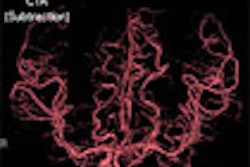
Thin sections also increase the difficulty of separating vessels from nodules, Mendel said. On a thick-section image, vessels and nodules retain their linear appearance, but as sections become thinner, the cross-section of a nodule and vessel grow more similar in appearance.
The MIP alternative
Maximum intensity projection (MIP) images, an old standby, are a reasonable alternative to CAD for CT lung studies, according to Mendel. They solve the nodule visualization problem in thin-section images by making vessels appear linear without changing the appearance of nodules, he said. One caveat: MIPs artificially increase the apparent size of lung nodules, so it's essential to go back to the original slice data for measuring them.
But MIPs reduce error rates and reading times, and perhaps best of all, they're available on almost every standalone workstation. Why aren't MIPs used more often? Just like CAD, most aren't integrated into PACS, Mendel said.
"Why CAD? What's the cost of a missed pulmonary nodule in patient care, to you, and maybe your patient's attorney?" Mendel asked with rhetorical flourish. "Do you have the time to really look over CT scans in detail and find those nodules? Are you going to be inundated with more and more studies where early detection and screening is going to be your primary mission?"
It would appear so. More detected nodules mean higher exam volumes and more follow-up exams. Better ways are needed to follow detected nodules over time and CAD could help, Mendel said. Finally, a lot of CT scans are acquired not specifically for lung evaluation -- but which contain lung data -- and there needs to be a way of looking at these images, too.
CAD in the corner
Of course, PACS makes lung CT reading faster and more efficient all by itself. People like cine review; side-by-side images make comparison easy, Mendel said. It is also true that PACS may be exacerbating the data deluge because there's no limit on the number of slices, no need to worry about film costs, no limit on the ways CT data can be manipulated for review, and the images last forever, Mendel said. By and large, however, PACS' effect on lung exams is positive. The problem is that most lung CAD systems are stuck in the corner of the room, unconnected to PACS, he said.
Workflow integration
At Mendel's practice, a lung exam with MIPs is fully integrated into the workflow. Images are sent from the CT scanner to the PACS, reconstructed, read, and reported. But CAD requires an awkward sort of bypass operation.
"I have to go to a workstation to use it, I have to figure out where the nodules are, I have to send it back through the PACS," Mendel said.
Loading the CAD software on the PACS doesn't help much because it still has to be launched on a separate window, so it's not really integrated into the workflow, Mendel said. A first step toward integration might be to have the CAD output sent to PACS as a data overlay. But this won't make CAD usable like full integration, whereby:
- CT data are acquired and sent to the PACS workstation.
- PACS reads the associated CPT code for the study (for example thoracic spine) and determines that there is lung data to be read.
- Lung data are sent to CAD automatically and analyzed.
"When you go to read the study, those CAD tools are available to you the same way the ROI and distance measurements are available (now)," Mendel said. "You simply click on the nodule and the work's done for you. And this gets me back to that nice linear workflow."
Medicolegal issues
Mendel noted that much has been written about medicolegal issues associated with CAD. Radiologists have questioned the need to save nonactionable CAD marks, fearing malpractice suits in the future when CAD findings that were dismissed by the radiologist are inevitably linked to future cases of lung cancer. At this point the question of to save or not to save CAD records is being answered by others, Mendel said.
"The CMS (Centers for Medicare and Medicaid Services), the FDA, and insurers are fixing that problem for us," Mendel said. "I've read two legal opinions that say CAD output is a medical record. We're probably stuck keeping it forever."
On the other hand, keeping CAD records may not be the legal liability it was once feared to be, he said, referencing a 2004 paper in Radiology.
"They're saying that CAD is a diagnostic tool we're using, and that there's a good legal argument that even if we see something on CAD and dismiss it, that we're better having the CAD output there so we can show we did that extra step (to) provide the best patient care," Mendel said. "So from their point of view CAD marks are medicolegally neutral and may even help."
The authors, Dr. Debra M. Ikeda and colleagues explained the mammography CAD study as follows:
"The CAD mark is intended to draw the radiologist's attention to a given area, and is used to mitigate the possibility of detection error in case the anatomic site of concern has not been sufficiently evaluated," they wrote. "Once an area is identified, either with or without a CAD mark, the decision to recall the patient is based on the radiologist's training, familiarity with signs of breast cancer, and experience. This decision is subject to the legal test of reasonableness -- not of accuracy or certainty -- so that a mistake is not tantamount to breaching the requisite standard of care" (Radiology, March 2004, Vol. 230:3, pp. 811-819).
"Our study results indicate that CAD systems mark a finite percentage of nonspecific mammographic findings in areas where cancer subsequently develops," the authors continued. "However, that percentage is neither sufficiently high nor designed for specificity to the extent that it can be an independent variable in deciding the reasonableness of recall. Similarly, if a finding that would be reasonable to recall is not recalled, then the presence (or absence) of a CAD mark is subordinate to the analysis of the specific mammographic features of that area."
CAD penetration
Another reason why CAD has not been incorporated into PACS networks is that the vendors are busy fielding large volumes of requests to improve their software. But if radiologists start telling PACS vendors they're missing nodules and they need a tool like lung CAD to be incorporated, "they'll do it for us even ... without (CAD) reimbursement," Mendel said. CAD vendors are doing their part by getting reimbursement and the like. "But we need to be driving force," he said.
There's another reason why lung CAD has languished, Mendel said. In contrast to the public displays of compassion mounted for breast cancer sufferers, lung cancer has no 10K races, no colored bracelets urging a fight for the cure.
"And when you think about the issues that brings up in terms of politics and healthcare, you can understand why the adoption of lung CAD is a little slower than mammo CAD," he said.
By Eric Barnes
AuntMinnie.com staff writer
August 24, 2006
Related Reading
Pulmonary nodule decisions must be individualized, August 16, 2006
Canadian lung CAD cuts false positives, July 24, 2006
CAD improves lung nodule detection, June 1, 2006
Part II: Automated CT lung nodule assessment advances, May 16, 2006
Part I: Automated CT lung nodule assessment advances, April 17, 2006
Copyright © 2006 AuntMinnie.com