Multidetector CT is a mainstay modality for evaluating urinary conditions, from hematuria and urolithiasis to urinary tract infections, and from renal masses to trauma imaging. It helps that the newer scanners enable image acquisition in a single breathhold, and a combination of enhanced and unenhanced scans can be made to look a lot like intravenous urography in coronal images acquired during the excretory phase.
The problem is that no matter what modality is used to image the entire collecting system, peristalsis makes it "difficult to obtain a single image in which all urinary tract segments are opacified and distended," wrote a research team from Brigham and Women's Hospital in Boston. For this reason contrast agents are often supplemented with intravenous saline, which has been found to improve opacification of the collecting system and ureters.
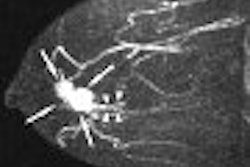
"Despite these findings, some patients' ureters may still not be fully opacified or distended," wrote Dr. Stuart Silverman, Dr. Syed Akbar, Dr. Koenraad Mortele, and colleagues in the September issue of Radiology. The group retrospectively evaluated whether administration of intravenous furosemide, either alone or in addition to intravenous saline, improved the depiction of the normal urinary collecting system at multidetector row CT urography (Radiology, September 2006, Vol. 240:3, pp. 749-755).
The study reviewed excretory-phase MDCT images from 87 patients (44 women and 43 men ages 21-83, mean 53). In addition to contrast media, the exams were performed with 250 mL of intravenous saline alone (n=35), both 250 mL of saline plus 10 mg of intravenous furosemide (n=26) or using 10 mg of furosemide alone (n=26).
Images were acquired on either a four- or 16-detector Somatom CT scanner (Siemens Medical Solutions, Malvern, PA) in a three-scan protocol. For the four-detector scan, the abdomen and pelvis were imaged at 2.5-mm collimation, pitch 1, 120 kVp, and 155-200 mAs. The kidneys were imaged during the nephrographic phase 100 seconds after IV administration of 100 mL iopromide at 3 mL/sec with 2.5-mm collimation, pitch 1-1.25, 120 kVp, and 155-200 mAs, the authors wrote.
For those patients receiving furosemide (Lasix, Abbott Laboratories, Abbott Park, IL) the agent was administered 2-3 minutes before the contrast. Excretory-phase images were acquired 15 minutes after contrast injection at 1.0-mm collimation, pitch 0.65-1.00, 120 kVp, 165-185 mAs.
The 16-slice scans used the same contrast protocol and the following settings -- for the unenhanced scan: 1.5-mm collimation, pitch 0.875, 120 kVp, 160-280 mAs; for the nephrographic phase the figures were 1.5-mm collimation, pitch 0.875, 120 kVp, and 160-280 mAs; and for the excretory phase the settings included 0.75-mm collimation, pitch 0.82-1.00, 120 kVp, 160-280 mAs.
The excretory-phase images were reconstructed transversely with 5-mm-thick sections at 5-mm increments, and coronally with 3-mm thick sections at 3-mm intervals. Maximum intensity projections and curved planar reformats were also reconstructed.
"Three readers, blinded to the imaging technique used, individually assigned opacification scores (0-3 scale, 3 indicating complete opacification) to each of six urinary collecting system segments," the group wrote. "Urinary distension was assessed by one reader by measuring transverse widths of the proximal, middle, and distal ureter segments."
According to the results, furosemide produced higher mean opacification scores in all segments except the pelvis, where saline yielded better opacification.
In the middle ureteral sections, the mean opacification scores achieved with furosemide (2.60 for the right side, 2.71 for the left) were significantly higher than those achieved with saline (2.20 for the right side, 2.26 for the left, p <= 0.008). The same was true for the distal ureteral segments: higher with furosemide (2.56 for the right side, 2.71 for the left) compared to saline (1.37 for the right side, 1.72 for the left, p < 0.001 for both).
"However, in both renal pelves, the mean opacification scores were significantly higher when multidetector-row CT urography was performed with saline (2.95 for the right side, 2.90 for the left) than when it was performed with furosemide (2.72 for the right side ([p < 0.001], 2.69 for the left [p < 0.02])," the group wrote.
No overall benefit was seen by administering both saline and furosemide. In fact, the mean maximum width of the left middle ureteral segment was significantly higher with furosemide alone (5.96 mm) than with both (4.90 mm, p = 0.01), according to the authors.
Furosemide significantly improved middle and distal ureteral opacification compared with saline, and it improved overall distension. Only the renal pelves did better using saline, or using both furosemide and saline.
"The mechanism of action of furosemide involves inhibition of sodium chloride reabsorption in the renal thick ascending limb of Henle, with a subsequent decrease in fluid reabsorption in the renal medulla," Silverman and colleagues explained. "Two features that distinguish saline-induced diuresis from furosemide-induced diuresis are (a) saline increases glomerular filtration rate, while furosemide does not increase and may even decrease glomerular filtration rate to a small extent and (b) furosemide increases urine flow rate more promptly and to a greater extent than does saline, particularly in a 'water-loaded' subject. Therefore, because contrast medium is mostly filtered, saline increases opacification of the collecting system by increasing contrast medium excretion." And by increasing flow rate, they continued, furosemide decreases urinary transit time except in the pelves, which have greater capacity.
The authors said they believe that as a result of higher flow rates, furosemide increases opacification by delivering more contrast medium to all segments.
"Our data suggest that the predominant factor in ureteral opacification was decreased transit time rather than differences in the amount of contrast medium filtered among the different protocols," they added.
Using a split contrast dose is advantageous relative to the study protocol because it reduces the number of scans from three to two, the team noted. There is a theoretical downside in that by splitting the dose, less contrast is available to create a nephrogram and less to opacify the collecting system.
"However, the former issue could be overcome by using a higher dose of contrast medium, and the latter issue could be overcome by adding furosemide to the regimen," they wrote.
Finally, the authors said they believe furosemide is probably safe. Two cases of minor urticaria appeared to result from the contrast medium rather than the furosemide, and moreover, no reactions have been seen in the department while using furosemide with MRI or nuclear medicine exams.
Furosemide is now part of the routine protocol; the use of saline at the facility is now reserved for patients with allergies to furosemide or sulfa drugs, and for those with systolic blood pressure of < 90 mm Hg, the team wrote.
By Eric BarnesAuntMinnie.com staff writer
September 8, 2006
Related Reading
CT urography useful in diagnosing bladder cancer, August 22, 2006
MDCT makes inroads in urology, biopsy guidance, and oncology imaging, June 19, 2006
Zero to 64: CT urography zooms ahead with more detector rows, March 18, 2005
CT gains ground in urology, June 18, 2004
Copyright © 2006 AuntMinnie.com