An international group of researchers said they have encouraging preliminary results from the use of dynamic contrast-enhanced MRI (DCE-MRI) to help determine the malignancy of cancer cells in the protective sac -- the mesothelium -- that surrounds most of the body's internal organs.
Mesothelioma -- a form of cancer that attacks the mesothelium -- is often fatal. Treatments such as surgery, chemotherapy, and radiation "frequently yield unsatisfactory results," with a median survival rate of six to 12 months, the report stated in Chest, the journal of the American College of Chest Physicians (Chest, June 2006, Vol. 129:6, pp. 1570-1576).
The National Cancer Institute attributes most mesothelioma cases to the inhalation of asbestos particles, though the disease may take 20 to 50 years to develop after exposure.
The study reviewed 19 patients diagnosed with malignant pleural mesothelioma (MPM) and who were scheduled to receive chemotherapy with gemcitabine, an antimetabolite used to stifle growth and destroy cells in various forms of cancer, including that of the pancreas, breast, and lung. A potential side effect of gemcitabine is that it also may adversely affect the growth of normal cells and contribute to hair loss.
However, additional therapeutic options are coming to caregivers with newer drugs, making the effort "essential to advance noninvasive imaging technologies that can map out in vivo pathophysiologic characteristics of MPM...to assess the biological response to new therapies that might impact disease survival," wrote lead author Dr. Frederik Giesel from the German Cancer Research Center in Heidelberg. Giesel's co-authors included Dr. Michael Knopp, Ph.D., from Ohio State University in Columbus.
Modalities' value
While CT has been used for diagnosis, staging, and monitoring therapeutic response to MPM, the report cited preferences for MRI in its analysis, adding that CT can be "misleading" in evaluating the extent of disease. FDG-PET has not been used widely in cases of MPM, because of cost, limited availability, and inability to provide adequate anatomical information. The combination of PET-CT has improved the ability to detect MPM in patients, but the German researchers opined that PET-CT systems are expensive, and other functional imaging modalities, such as DCE-MRI "might be of benefit in this setting."
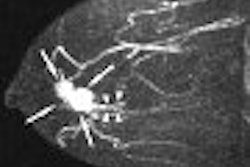
DCE-MRI acquires images sequentially during intravenous administration of a gadolinium chelate. The passage of contrast media through tissue, the study added, "can be used to assess and map out differences in microcirculation and vascular permeability."
In some cases, DCE-MRI has enabled earlier predictions of positive response to chemotherapy.
All 19 patients were diagnosed with either stage II or stage IV MPM and were included in the clinical trial with single-agent chemotherapy and a standard 1.5 Tesla MRI. DCE-MRI was performed prior to chemotherapy and again after the third and sixth cycles of therapy. Seven of the 19 patients were scanned on all three occasions.
The analysis concluded that "parametric mapping based on DCE-MRI in MPM depicts not only the lesion and its extent, but can map out the heterogeneity of microcirculation within the full thoracic extent of MPM."
The technique shows its best results when the protocol includes shallow breathing, shorter image acquisition time, and adjusting the contrast injection rate to compensate for respiratory and cardiac motion during repetitive image acquisitions. The technique provides a noninvasive insight into tumor microcirculation and vascular permeability, as had been anticipated, prior to and during therapy.
Tempering expectations
The imaging modalities may play a key role in identifying candidates for particular therapies, the authors stated, but they also cautioned that while the preliminary results are encouraging, the findings have some limitations.
One consideration is the study's small sample size of 19 patients. The report also noted that MPM is "relatively uncommon," so several patients did not complete the imaging due to the progression of disease, while a few other patients were unable to complete all three scans. Also, the technique did not use the most rapid MRI technology available today, as researchers had "to fix the technique for the duration of the study, which took several years to accrue."
By Wayne ForrestAuntMinnie.com staff writer
September 15, 2006
Related Reading
Report links asbestos to larynx cancer, June 8, 2006
Higher lung cancer risk seen in asbestos-exposed smokers, November 28, 2004
Part II: A survey of asbestos-related imaging, September 4, 2004
Separating inflammation from malignancy on thoracic FDG-PET, April 9, 2004
Copyright © 2006 AuntMinnie.com