ARLINGTON, VA - Trial results unveiled today marked the apparent end of a long road to validation for virtual colonoscopy (VC or CT colonography [CTC]), a radiology-based colon screening exam whose advocates have toiled for more than a decade to show equivalent detection sensitivity in a large screening trial compared to more invasive optical colonoscopy.
Preliminary results of the National CT Colonography Trial (ACRIN 6664), a study funded by the National Institutes of Health (NIH) and performed on 2,531 participants in 15 U.S. centers, yielded an impressive per-patient sensitivity of 90% for adenomatous colorectal lesions 1 cm or larger in diameter, a sensitivity on par with that of optical colonoscopy.
Optical colonoscopy retains the considerable advantage of being both diagnostic and therapeutic, in that colorectal polyps can be removed concurrently with their detection. Nevertheless, reported principal investigator Dr. C. Daniel Johnson from the Mayo Clinic in Rochester, MN, only 8.3% of trial participants would have proceeded to same-day optical colonoscopy for removal of polyps 6 mm or larger, a referral rate low enough to suggest that VC will not be too expensive an alternative for routine use in colorectal cancer screening. Inasmuch as optical colonoscopy served as a reference standard for the comparison of VC trial results, 100% of the participants were referred for the exam immediately after VC.
"Colon cancer is the second most common cancer killer in the U.S., affecting one in 18 individuals in the United States," Johnson said, adding the latest grim statistics: 145,290 new cases in 2007, and an estimated 73,470 deaths. Yet only one-third to one-half of the 70 million people eligible to screen in the U.S. ever get tested. It is hoped that the addition of a new alternative will encourage more individuals over 50 years of age to get screened, though as in optical colonoscopy, most VC patients will still have to undergo cathartic bowel cleansing before screening.
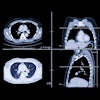
"From a patient perspective, once the colon's prepped, it's pretty easy, just two breath-holds in the prone and supine position, and then the examination is done on the image data rather than on the patient," said Johnson, a professor of radiology at the Mayo Medical School in Rochester, MN. He presented the first results of the trial at the 2007 ACRIN (American College of Radiology Imaging Network) fall meeting.
The efficacy of colorectal cancer screening has already been proved because it can detect precursor lesions in the colon long before they progress to cancer, Johnson said. The problem with VC as a screening alternative has been the variability of multicenter trial results. While Pickhardt et al demonstrated 94% sensitivity and 96% sensitivity for significant colorectal lesions in more than 1,100 asymptomatic subjects in 2003, subsequent studies by Cotton et al and Rockey et al yielded sensitivities as low as 55% and 59%, respectively, for clinically significant polyps. These later results cast serious doubt on the robustness of VC as a screening method, though many radiologists maintained that poor study design and lack of training were the main problems.
"The aim of this (ACRIN) study was to evaluate the sensitivity of CT colonography for detecting participants with at least one adenoma a centimeter or larger using colonoscopy as the reference standard," Johnson said.
The 15 U.S. sites included both academic centers and private practices, which recruited 2,600 asymptomatic outpatients who were scheduled for optical colonoscopy screening. Those with symptoms suggestive of an elevated risk of colon cancer, such as blood in stool, abdominal pain, or family or personal history of colorectal polyps, were excluded from the study.
Training was an important component of the study, with VC readers obligated to have read at least 500 cases, or attend a 1.5-day training course. And all had to pass a certified exam in which they detected at least 90% of the adenomas 1 cm or larger in 50 cases, Johnson said.
"It's interesting to note that more than half of the readers had to undergo additional training in order to pass the certified exam initially, and with additional training, all the readers eventually passed," he said.
Stool tagging began 24 hours before imaging with the ingestion of 16 grams of barium sulfate in three doses with meals, Johnson said. This was followed the evening before VC with a cathartic prep and residual fluid tagging with 60 mL of a water-soluble iodinated contrast agent. All subjects received 1 mg of glucagon 10 minutes prior to mechanical colon insufflation with CO2.
After insufflation, prone and supine CT images were acquired on scanners representing each of the major vendors with a minimum of 16 detector rows. Thin-section images were acquired at 0.6-mm to 1.25-mm collimation with reconstructions at 0.8- to 1-mm intervals, using a low-dose protocol of 50 mAs. Colonoscopy was performed on the same day in 99% of the cases by experienced staff gastroenterologists, who were blinded to the VC results.
A central pathology laboratory examined the results of all polypectomies, and segmental unblinding of VC results for the gastroenterologists was not used. A lesion matching process was used to compare VC detections to colonoscopy findings. In order for a polyp detected at VC to be counted as a true-positive, it had to match a conventional colonoscopy finding in the same colonic segment and within 50% of the size reported at VC.
From a total of 2,600 subjects, eight were deemed ineligible, 10 withdrew from the study, 42 had incomplete colonoscopy, and nine had incomplete VC, leaving a total of 2,531 or slightly more than 97% of the total who completed the study, including 1,205 men and 1,362 women with an average age of 58 years, Johnson said. About 10% (n = 248) had an increased risk of colon polyps due to personal or family history of colon polyps, he said.
More than half of the studies were performed on 64-detector-row scanners, and were interpreted in either primary 2D or 3D reading on software from several major vendors.
Overall there were 547 polyps in 390 patients 5 mm or larger in size, 392 polyps 6-9 mm in 258 patients, and 155 lesions 1 cm or larger in 132 patients, Johnson said. The mean diameter was 8.9 mm, distributed as follows: right colon (29%), transverse colon (17%), left colon (38%), and rectum (16%).
A total of 374 of the 547 (68%) colonoscopy-proven lesions were adenomatous polyps or cancers, including 128 lesions 10 mm or larger in 109 patients (4.3%), and seven carcinomas 5 mm or larger in diameter, Johnson said.
The chart below shows VC's sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for detecting patients with adenomas ranging in size from 5 mm or larger to 10 mm or larger.
|
"You can see that (VC) sensitivity remained high, 84% or more, for polyps 7 mm or larger," Johnson said. "Specificity remained high, 86% to 89%, across all lesions." The area under the curve rose from 80% to 90% for adenomas 5-10 mm in size.
Even the rigorous per-adenoma sensitivity measure was 59% (≥ 5 mm), 70% (≥ 6 mm), 75% (≥ 7 mm), 80% (≥ 8 mm), 82% (≥ 9 mm), and 84% (≥ 10 mm).
Interobserver variability was "actually quite tight," Johnson said, and seven of the 15 readers detected 100% of the polyps. Interestingly, the overall sensitivity difference between primary 2D reading (87%) and primary 3D reading (88%) was not statistically significant, he said. And 3D took almost six minutes longer to review on average, at 25.5 minutes versus 19.4 minutes for primary 2D. The various software packages used for interpretation did not yield significant differences in sensitivity either, Johnson added.
"I think we can say that CT colonography is similar to the performance of colonoscopy for large adenomas 1 cm or larger, as well as those intermediate adenomas 5-10 mm in diameter," Johnson said. "And I think it's reasonable to consider broader application of this relatively noninvasive imaging modality, which hopefully will enhance compliance with colorectal cancer screening guidelines. The prevalence of those adenomas 6 mm or larger was 8.3%; this would indicate that most patients undergoing CT colonography wouldn't need colonoscopy, sparing them the cost, risk, and inconvenience of that second test."
The contributions of reader training and advanced techniques in the success of the trial cannot be underestimated, Johnson said. The success in the past has been attributed to the primary 3D reading technique, but the results showed that primary 2D can be as accurate. In addition, the study was performed with a low-dose CT technique yielding a total dose of about 5 mSv per exam, an amount the Health Physics Society considers a risk that is either nonexistent or "too small to be measured," he said.
Johnson said he expects the information to be of interest to the health agencies that define the tests that are included in colorectal screening guidelines, and called on the primary care and gastroenterology communities to work together with radiologists to prepare for the wider implementation of CT colonography for screening.
"I think the results show a remarkable amount of thoughtful effort" on the part of the researchers, commented Dr. Elizabeth McFarland, adjunct professor of radiology at the Mallinckrodt Institute of Radiology at Washington University in St. Louis. What matters from this point forward is "how we disseminate this (modality) in a way that we maintain high standards and make it feasible for people to do out in the community," she said.
"Let's all agree that the validation phase is over, and let's work on widespread screening," said Dr. Perry Pickhardt, an associate professor of radiology at the University of Wisconsin in Madison, in a telephone interview with AuntMinnie.com.
The 25-minute 3D reads "are almost triple our current reading times" using different software, added Pickhardt, a proponent of primary 3D reading. "But I'm not worried about the whole 2D/3D issue. People will find out on their own which method works best for them," he said. "The numbers are really good, and overall it's good news."
By Eric Barnes
AuntMinnie.com staff writer
September 28, 2007
Related Reading
Gastroenterologists plan to perform VC, January 25, 2007
Colonoscopy declines at VA: Is limited capacity to blame? November 13, 2006
New data reveal higher efficacy for primary VC screening, October 18, 2006
VC finds risky polyps, might reduce polypectomies, June 8, 2006
Radiologists eye VC practice post-ACRIN, February 10, 2007
Copyright © 2007 AuntMinnie.com