Pulmonary embolism (PE) rule-outs can be done with half the normal contrast dose using dual-energy CT (DECT) -- on a single-source scanner. Researchers from Canada believe their new protocol is robust enough to open up a critical diagnostic test to patients who weren't candidates for CT pulmonary angiography (CTPA).
In a prospective randomized study, dual-energy CT delivered equivalent image quality, signal-to-noise ratios, and radiation dose compared to standard CTPA using less than 30 mL of contrast media.
PE is a common condition resulting in approximately 250,000 hospitalizations or deaths each year in the U.S., and it's the third largest cause of cardiovascular mortality, said Jonathon Leipsic, MD, from St. Paul's Hospital in Vancouver, British Columbia, in a presentation at last month's RSNA meeting. But owing to typical iodinated contrast doses of up to 100 ccs, he said, patients with renal insufficiency are frequently ineligible for the gold standard, CT pulmonary angiography, and must undergo other tests, such as the ventilation/perfusion (V/Q) scan, that may not be as effective for ruling out PE.
"Dual-energy CT, which was introduced on the dual-source CT scanner and more recently with rapid kV switching on a single-source scanner, has potential to increase the signal in the vascular bed by reconstruction of images at lower monochromatic energies closer to the k-edge of iodine," Leipsic explained. "This affords us an opportunity to reconstruct images at higher monochromatic energies paralleling the routine 120-kVp exam, enabling a complete evaluation of the pulmonary parenchyma and soft tissues as well."
In their study, the researchers from Vancouver, along with colleagues at the University of Washington in Seattle, prospectively enrolled 68 consecutive patients with body mass index (BMI) less than 35 kg/m2. Patients were randomized to dual-energy CTPA (Discovery CT750 HD, GE Healthcare, Chalfont St. Giles, U.K.) (n = 35) using half-strength IV contrast (50% saline) or routine CTPA using full-strength contrast.
The CT scanner's dual-energy spectral imaging protocol was combined with image reconstruction at 50 kVp for evaluating the vascular bed and 70 kVp for the pulmonary parenchyma using a dilution of 1:1 contrast and saline. A timing bolus was used for both cohorts, and a standard calculation was used to determine contrast volumes. The standard protocol scan parameters were 100 kVp for patients with BMI less than 30 and 120 kVp for those with BMI greater than 30, with a noise index of 28.
Both protocols began with a timing bolus to determine scan delay and contrast volume, Leipsic said. The standard protocol contrast injection volume was 50-80 cc of contrast at 4 cc/sec. Volume for the reduced-contrast cohort was identical but the contrast was diluted 50:50 with saline, he said. Dual-energy images were reconstructed and analyzed at a monochromatic energy of 50 kV, close to the k-edge of iodine.
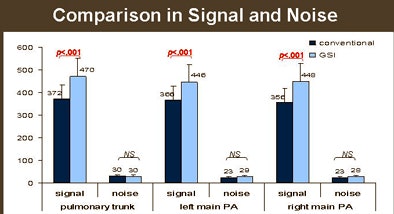
Signal was measured (mean region of interest) at the left pulmonary, left apical, and right posterior basal arteries. Contrast was measured as a mean signal in the arteries and in the pectoralis. Noise was measured as a standard deviation of signal in the main pulmonary artery. Signal- and contrast-to-noise ratios were calculated.
Image quality was evaluated by two radiologists independently using a three-point Likert scale to assess image quality (3 = very good, 2 = diagnostic, 1 = nondiagnostic), "with focus given to the confidence in diagnosing and excluding PE to the segmental level," Leipsic said.
"The study populations showed no statistically significant differences in age, height, weight, or BMI, but both cohorts were overweight with a median BMI of 27," he said.
"We saw a statistically significant reduction in contrast volume injected" (median 28 ccs in the DECT protocol versus 62 ccs in the standard protocol [p < 0.001]) "without compromising the dose-length product," Leipsic said. The mean dose-length product was 406 in the conventional protocol versus 419 (p = NS) in the DECT protocol (equivalent to approximately 6.5-6.8 mSv, depending on the conversion factor).
Contrast and noise were also similar for both protocols. In fact, the signal-to-noise and contrast-to-noise ratios were slightly higher for the reduced-contrast cohort, Leipsic said.
 |
| Signal-to-noise ratios (SNR) and contrast-to-noise ratios (CNR) were similar for reduced-contrast and conventional PE protocols. All images courtesy of Jonathon Leipsic, MD. |
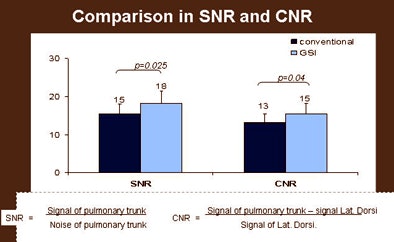 |
In reconstructing monochromatic images at 50 kV, there was a statistically significant improvement in overall vascular bed signal, both in the left pulmonary artery and right main pulmonary artery, without a statistically significant increase in noise. "And not surprisingly, we saw a statistically significant increase in the signal-to-noise ratio," Leipsic said. The contrast-to-noise ratio measured the difference between the pulmonary circulation and the latissimus dorsi for calculation of contrast.
Similarly, radiologist assessment of image quality showed no significant differences between the low-dose (mean score of 3.0 on the Likert scale) and standard (mean score of 2.95) protocols.
"There was a trend toward some inferiority in our contrast-reduced protocol, largely in our very obese patients," he said. "The most obvious limitation to our data is that recruitment is limited to patients with BMI less than 35," he said. "In our first 68 patients, we had three cases that were considered nondiagnostic and two that were suboptimal by one of our readers, but all of these patients were obese with BMIs greater than 32.5," he said.
The study is ongoing, and as of mid-January 2011, 109 patients had been scanned, Leipsic told AuntMinnie.com by telephone this week.
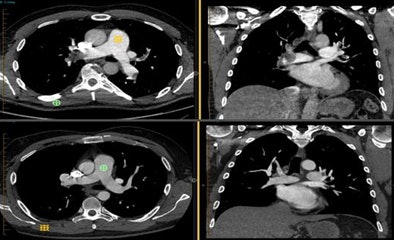 |
| No differences in image quality are perceived between the two protocols. (Top row) 62-year-old man with acute onset of chest pain underwent a reduced-contrast spectral dual-energy protocol: 50 kV, signal-to-noise ratio = 17:1, contrast-to-noise ratio = 14:1, and 22 cc of iodinated contrast. (Bottom row) 58-year-old man with new-onset dyspnea received a conventional PE rule-out protocol: 100 kV, signal-to-noise ratio = 14:1, contrast-to-noise ratio = 12:1, and 50 cc of iodinated contrast. |
"Reduced contrast DECT pulmonary angiography is feasible in patients -- certainly between BMIs of 25 and 32 -- showing noninferiority in noise and signal properties as well as qualitative image quality measures," he said. "We would suggest that a median contrast volume of 28 ccs in overweight patients with a median BMI of 27 with diagnostic image quality has at very least the potential to broaden the scope of CTPA to include patients with renal impairment."
In response to a question from the RSNA audience, Leipsic said the protocol was not for everyone with suspected PE.
"No one is suggesting that this should be done routinely, but what we're trying to do is prove a concept such that patients who come to the lab with [ejection fractions] of 35 that previously were never candidates for CTPA, and elderly patients with parenchymal lung disease that we were not comfortable imaging -- with contrast volumes of 25 ccs, we can consider those patients candidates for the gold standard CTPA."
How many more patients could be scanned if only severe renal insufficiency were sufficient to ban CT? Leipsic said he suspects patients are steered away from CT quite frequently, but says supporting data are hard to come by.
"We lack some of that data," Leipsic told AuntMinnie.com. "Once patients have renal insufficiency, they will not get referred for CT, there will be a referral bias, and they'll have to pursue other tests [such as a V/Q scan] because referring docs won't even consider them a candidate."
By Eric Barnes
AuntMinnie.com staff writer
January 14, 2011
Related Reading
Rate of imaging utilization in emergency room escalates, January 3, 2011
Automated PE protocol tool optimizes contrast use, image quality, November 29, 2010
PE risk factor assessment reduces need for CT angiograms, June 16, 2010
Consider screening DVT patients for silent pulmonary embolism: review, May 14, 2010
Is imaging underutilized for diagnosing PE? March 31, 2010
Copyright © 2011 AuntMinnie.com




















