Patients with a family history of coronary heart disease should pay heed to their coronary artery calcium (CAC) scores to boost their chances of living longer, says a new study of more than 40,000 patients.
The massive U.S. trial found that increasing CAC scores were more strongly associated with mortality in patients with a family history of coronary heart disease, compared with others at similar risk without a family history.
"I think this shows something a little bit unique from how we stratify patients now," said co-investigator Dr. Matthew Budoff in an interview with AuntMinnie.com.
Currently, in the Framingham heart disease risk score model, family history is not a risk factor, said Budoff, a professor of medicine at the University of California, Los Angeles (UCLA). "This study shows that family history is actually an important risk factor and should probably be considered in the risk models," he said.
The study was presented by Dr. Kerunne Ketlogetswe, from Johns Hopkins University, earlier this month at the American College of Cardiology (ACC) meeting in New Orleans. It included some 44,052 individuals at U.S. centers including Johns Hopkins, UCLA, and Cedars-Sinai Medical Center -- following some patients for as long as 13 years. In all, 10 leading U.S. institutions collaborated in the study.
Patients with a family history of heart disease are known to have a higher burden of atherosclerosis than others with similar demographics. And the presence of CAC is strongly correlated with the magnitude of coronary plaque burden and with the development of subsequent coronary events.
Previously, the Multi-Ethnic Study of Atherosclerosis (MESA) found a higher odds ratio of having measurable CAC among patients with a family history of heart disease. In that study, 44% of participants reported a family history.
However, it's unknown whether the increased calcification burden translates into higher rates of cardiac events and deaths -- a question probed by the Johns Hopkins team.
"We wanted to establish whether family history was an important risk factor, and we wanted to establish that information related to family history was incremental to calcium scores," Budoff told AuntMinnie.com. All-cause mortality was the primary end point in the study.
Beginning in 1990, the group began screening patients for coronary artery disease using calcium scoring with electron-beam CT (EBCT) (Imatron Ultrafast CT scanner models C100 or C150, GE Healthcare). Patients were followed for a mean of 5.6 ± 2.6 years (range, 1-13 years), with 100% follow-up. CAC scores were calculated using the Agatston method.
Patients were queried for basic demographic data and risk factors including age, gender, hypertension, dyslipidemia, diabetes, cigarette smoking, etc. They were asked whether they had a family history of heart disease, and were considered positive if any member of the immediate family had a history of myocardial infarction and/or coronary revascularization.
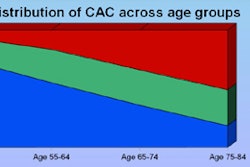
Over two decades, Ketlogetswe and colleagues examined 44,052 individuals without known coronary heart disease. In all, 16,402 (37%) of these individuals reported a family history of coronary heart disease.
Compared to patients without a family history, individuals with a family history were less likely to have CAC scores less than 400 (8% with family history versus 12% for others) (p < 0.0001).
Over the mean follow-up period of 5.6 ± 2.6 years, the group found an annualized mortality rate of 3.15 deaths per 1,000 person-years (95% confidence interval [CI]: 2.90-3.42) for those without a family history of heart disease, compared with 4.78 deaths per 1,000 person-years (95% CI: 4.30-5.31) for those with a family history.
All-cause mortality for patients with family history versus no family history
|
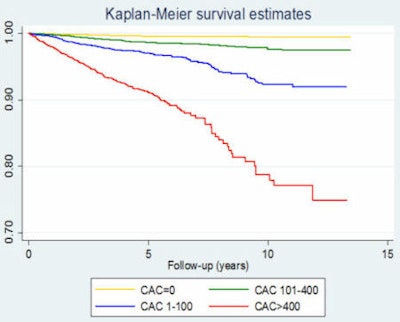
After adjusting for cardiac risk factors, increasing CAC scores (1-99, 100-399, and ≥ 400) were associated with increasing mortality, Budoff said. Still, increasing CAC scores were more strongly associated with mortality among those with a family history (hazard ratio, 2.87-9.86) than those without a family history of coronary heart disease (hazard ratio, 1.97-3.81).
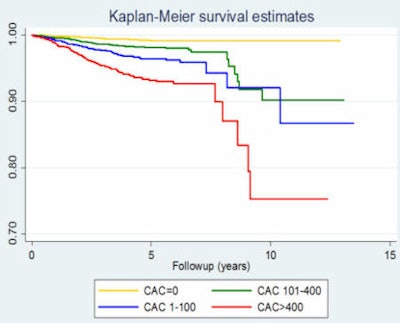 |
| Cox proportional hazards survival (n = 44,052) by electron-beam CT coronary calcium measurements in subjects with (above) and without (below) a family history of coronary heart disease. Results show that mortality increases more rapidly with increasing coronary calcium in patients with a family history of disease. Images courtesy of Dr. Matthew Budoff. |
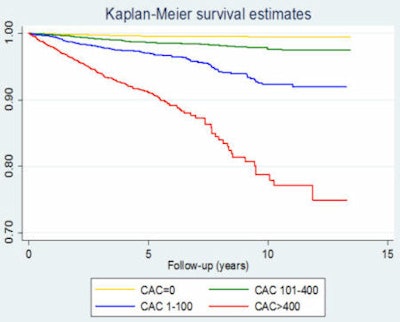 |
With some patients followed for as long as 13 years, the researchers found that the association between high calcium scores and mortality in the positive family history population "continues to get stronger as you go out further in time, so it appears that [CAC scoring] gives you long-term predictive power that gets more powerful over the years," Budoff said.
On a positive note, patients with a zero calcium score barely saw any increase in the risk of death even when they had a family history of disease. Cox regression analysis showed that a family history of coronary heart disease was associated with only a small increase in risk of all-cause mortality (hazard ratio, 1.53; 95% CI: 1.00-2.34; p = 0.05) in the lowest-risk individuals with zero calcium scores.
So for folks without calcium, "the mortality was basically identical with a family history," Budoff said. "It shows you that a calcium score of zero provides a long-term good prognosis -- regardless of other risk factors and regardless of family history."
The study confirms that CAC scoring can add quite a bit of useful information to the risk profile, particularly for the 58% of patients with a family history "who either have some or a lot of coronary calcium and their prognosis may not be as good," Budoff said.
So should everyone with a family history of heart disease get a coronary calcium score?
"Atherosclerosis is a completely treatable disease, so getting the information and giving it to the patient is going to add the ability of earlier treatment and more aggressive treatment for those at risk," he said.
And if patients did know their scores, would they change their lifestyles? Research results on this question have been mixed.
"I really believe a picture is worth a thousand words," Budoff said. "As a preventive cardiologist, I really see patients improve their behavior and improve their lifestyle based on their knowledge of their calcium score."
Of course, this trial still had a lot of patients with zero calcium, which is, of course, not a compelling factor for changing risky behaviors.
"That you need a positive calcium score to change your lifestyle may be an obvious conclusion, but you have to study the right population," he said.
To attempt to change risk behaviors in large numbers of people at higher risk, what's needed is another trial that recruits a higher percentage of patients with positive calcium scores -- for example, a little older and with more disease -- Budoff said.
"I would probably study diabetics," he said, "because diabetics tend to have positive scores, they tend not to be the most compliant patients because there aren't a lot of meds, and you could really see a potential change [in risk behavior] if there is a change."
In fact, the researchers are currently working to convince the U.S. National Institutes of Health (NIH) that a trial of higher-risk patients to look at this question would be useful; they hope to find out if a positive CAC score leads patients to lose weight, get their diabetes under control, and pay more attention to taking their medications and the like. That project is ongoing.
"I also think the study emphasizes that we need to modify the Framingham model to include family history, and we're actually using our results to come up with what we're calling 'Framingham Plus,' which will include family history in the risk stratification to make it a better predictor," Budoff said.