Australian researchers have combined coronary CT angiography (CTA) and coronary artery calcium (CAC) scoring in a single scan, saving time and reducing CT radiation dose by at least one-third.
With the aid of prospective electrocardiogram (ECG) gating, reduced tube current, and other dose-reduction techniques, coronary CTA has been transformed in recent years from a relatively high-dose exam (18 mSv or more) to one that can be obtained in most patients at doses as low as 1 mSv to 5 mSv.
However, the practice of acquiring a separate CAC scan before contrast is injected and coronary CTA is performed -- as occurs in most coronary CTA exams -- adds somewhere between 0.8 mSv to 2.5 mSv of additional radiation.
That radiation dose and acquisition time is no longer necessary, researchers said last month in a presentation at the 2011 American College of Cardiology (ACC) conference in New Orleans.
"By getting the calcium score from the contrast-enhanced scan, you only need one scan instead of two, and the radiation dose of the protocol is reduced by 30% to 50%," wrote principal investigator Dr. James Otton in an email to AuntMinnie.com. "Given the number of scans being performed, this could save tens or hundreds of iatrogenic cancers per year. Our preliminary data ... show that the new technique is clinically equivalent to formal calcium score measurement."
In selected patients, physicians can get both calcium score and anatomy at less than 1 mSv, he said.
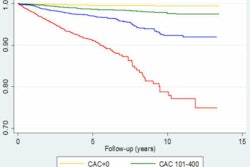
CAC is a powerful predictor of cardiovascular risk, providing quantitative prognostic information supplemental to both traditional Framingham risk assessment and coronary CT angiography.
Yet despite major reductions in the dose for coronary CTA, "the radiation dose of calcium score evaluation is largely fixed due to protocol constraints," the authors wrote in their poster presentation. "In some cases, calcium score scans now equal or exceed the radiation dose of contrast-enhanced CT coronary angiography."
Otton and his colleagues from St. Vincent's Hospital and the University of New South Wales, both in Sydney, along with investigators from Rigshospitalet in Copenhagen, Denmark, performed a prospective diagnostic accuracy study, comparing calcium estimates from contrast-enhanced coronary CTA to the reference standard of noncontrast calcium score CT. The results were validated and assessed for reliability in 100 patients.
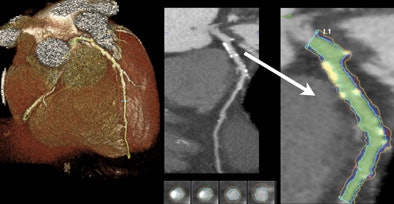 |
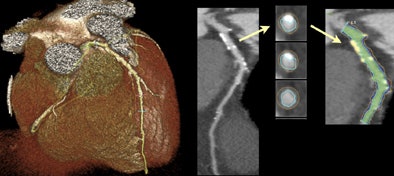
| Calcium can be readily identified on contrast-enhanced coronary CTA. After selecting an arterial segment with a software tool and making any necessary adjustments, the volume of high-intensity calcium can be measured. The calcium volume is converted to the Agatson score with a standard linear conversion factor. All images courtesy of James Otton. |
 |
The 100 patients included a broad range of body morphologies and clinical indications. Both 100-kV and 120-kV contrast CT scans were performed with identical accuracy. All scans were performed using a 320-detector-row Aquilion One CT scanner (Toshiba Medical Systems).
Scans and data were acquired from 100 consecutive patients undergoing both noncontrast CAC scoring and contrast-enhanced coronary CTA.
Eight patients were excluded for poor image quality, measured in excessive noise in the ascending aorta (HU standard deviation > 35), and two patients were excluded for the presence of a completely occluded coronary artery.
They identified calcifications by windowing and examining each axial slice in minimal slice thickness, as well as thick maximum intensity projection (MIP) and curved multiplanar reconstruction (MPR) views, Otton told AuntMinnie.com.
If an area of possible arterial calcification was seen, the calcium-containing arterial segment was selected in curved multiplanar view utilizing the SurePlaque plaque quantification software (VitreaFX v3.1, Toshiba).
The quality of automated arterial edge detection was also visually examined in arterial cross section reconstructed at 1-mm intervals along the arterial segment and was manually adjusted, as necessary, to include calcium deposits within the vessel wall and exclude luminal contrast.
The SurePlaque tool was adjusted to quantify the volume of high-intensity voxels exceeding 320 HU within the selected areas. The final Agatston calcium score estimate was obtained by multiplying the measured calcium volume by the empiric conversion factor.
Earlier studies showed that intramural calcifications could be measured from contrast-enhanced CT, Otton explained. But correlation was poor between mural elements above the lower Agatston threshold of 130 HU and both the noncontrast calcium score and traditional calcium volume measurements.
The inaccuracy occurs because noncalcified mural elements often occupy the range between 130 HU and approximately 200 HU, while at a voxel size of 0.5 mm3, whereas true calcified plaques generally greatly exceed 300 HU. After examining a range of thresholds, the group selected 320 HU.
A conversion coefficient was needed to convert the high-resolution high HU calcium volume measurement into the Agatston score. A derivation study showed the optimal conversion coefficient to be 3.13, the group reported.
SurePlaque was adjusted to quantify the volume of high-intensity voxels exceeding 320 HU within the selected areas. Once this volume was obtained, the final Agatston calcium score estimate was obtained by multiplying the measured calcium volume by the empiric conversion factor.
The method "has excellent accuracy when compared to the reference standard of traditional calcium score measurement," the authors reported. In addition, the results showed excellent inter- and intraobserver reliability.
Not only was the technique accurate across a broad range of patient types and scan parameters, but the tools required are readily available within commercial software packages.
The technique "appears suitable to replace traditional calcium scoring in combined calcium scoring and contrast-enhanced coronary CT protocols," Otton and colleagues wrote.
The associated radiation of calcium scoring is between 0.8 mSv and 2.5 mSv for modern-generation CT scanners, and may therefore exceed the total dose of contrast-enhanced CT angiography.
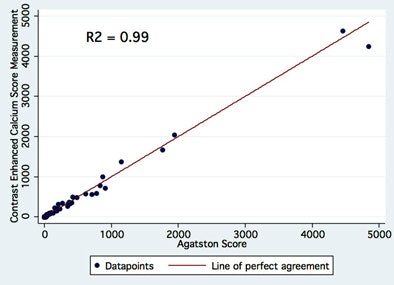 |
| Above, scatterplot of estimated versus measured calcium scores. The correlation is excellent both at high and low calcium scores. Below, difference in calcium score estimate and measured calcium score (Bland-Altman type plot). Also shown is the 95% reliability of traditional calcium scoring itself (from the MESA validation study -- Chung et al, AJR, 2008, Vol. 190). Almost all calcium score estimates lie within these limits. Both the inter- and intraobserver reliability of the new technique, as assessed by the intraclass coefficient, were 0.99. |
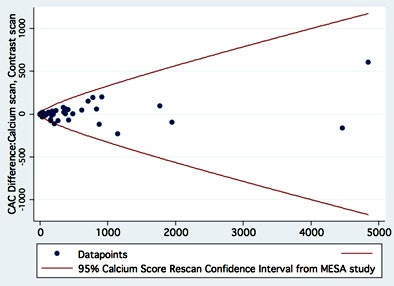 |
The results showed a range of measured calcium scores from 0 to 4,842. The resulting Pearson's coefficient (R2) of the regression of the two measurements was 0.99. Moreover, the accuracy of the technique to classify coronary calcium into standard risk and was near perfect (kappa 0.88). Finally, a Bland-Altman analysis showed nonsignificant bias, the authors reported. Both the inter- and intraobserver reliability of the new technique, as assessed by the intraclass coefficient, were 0.99.
The new technique is highly accurate compared to the reference standard of traditional calcium score measurement. Furthermore the technique has excellent inter- and intraobserver reliability and can potentially eliminate the practice of scanning each patient twice.
"While the dose of each scan is small, given the large and growing number of cardiac CT examinations, the ionizing radiation of calcium scoring, from a population perspective, is not insignificant," they wrote.
"In our cohort, the calcium score constituted 33% of the total received radiation dose and, had traditional calcium scoring been replaced by the proposed method, combined CT coronary angiography and calcium score estimation could have been performed at less than 1 mSv in selected patients," the researchers concluded.