CT has become increasingly popular for guiding interventional procedures such as needle placements, but these scans may be packing more dose than necessary. Researchers in China have found a way to cut the radiation dose by eliminating the need to perform multiple scans of the same area.
While CT is already the most commonly used modality for image-guided interventions due to its high image quality, the new method -- once optimized -- could go a long way toward making CT attractive for a wider range of procedures, according to researchers from Shanghai who presented their work at the 2011 Computer Assisted Radiology and Surgery (CARS) meeting in Berlin.
"CT has been widely used in many interventional procedures, but there is obviously concern about the radiation dose," said Dr. Jizhuang Zhang, from Siemens Shanghai Medical Equipment. "Dose in CT-guided interventional treatments is [unique] mainly because multiple repeating scans have to be performed. The question becomes, can we save dose by using redundancies?"
In CT-guided interventional procedures, CT is typically used to guide needle placement, necessitating multiple passes over the same anatomic territory, resulting in needless radiation exposure, Zhang explained. The proposed low-dose scan method eliminates the extra exposure without diminishing image quality.
Zhang and his Siemens colleagues Dr. Li Taotao and Dr. Wang Wei, all from the firm's CT research department, used the clinically relevant area around the interventional needle to set the region of interest (ROI) for repeat scans with the aid of an algorithm to select the optimal area.
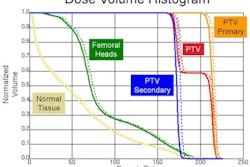
 |
| For a given ROI, there is always an optimal irradiation starting point, which is used to minimize the irradiation range and hence the radiation dose. For biopsies, the needle tip is tracked and a small area around the needle tip is selected as the ROI to be imaged. All images courtesy of Dr. Jizhuang Zhang. |
Once the new scan is complete, tissue within the ROI is rescanned and fused with the existing baseline image data. As the needle advances, the ROI is adaptively redetermined, based on the changing geometry of the ROI, Zhang said. The process includes the following steps:
- Preplanning of the needle path prior to intervention that incorporates scan times, needle movement, and additional needs of the procedure
- A full-dose scan before treatment to acquire and reconstruct baseline images
- Low-dose scans are acquired based on ROI geometry after the optimal start and end points of the exposure are calculated automatically
 |
Scans were completed in needle placement and biopsy cases, all of which spared at least 50% of the radiation dose compared with rescanning the entire region, Zhang said. For now, the ROI can be calculated manually or with the algorithm, which still needs some refinement.
"Calculation of the ROI can be performed manually -- the data can be defined by an experienced operator and ... calculated by the system," Zhang said. "By selecting the ROI, the new images will be obtained and will be fused with the previous images to generate the update. The updated images will also be used as reference images for the next scans."
 |
| The results show significant dose savings with the use of automated ROI selection. In biopsy (above), the irradiation varied from 156° to 165°, sparing 53% of the radiation dose compared with a traditional full-range scan. In microwave ablation (below), irradiation ranged from 156° to 172°, saving 51% of the dose compared with a full-range scan. |
 |
The method also works for CT guidance in microwave ablation of tissues, in which ROI selection is based on temperature monitoring, Zhang said.
 |
| In microwave tumor ablation, areas with high temperatures are selected as the ROI to be imaged to monitor spatial/temporal evolution of temperature distribution. |
The method has the potential for much more dose savings with the use of low-mAs imaging, motion correction, and other dose-saving techniques, he said.
In response to a question from the CARS audience, Zhang said that Siemens plans to introduce a commercial version of the method by the end of 2012.