Virtual and conventional colonoscopy were both beneficial but less cost-effective for preventing colorectal cancer than stool screening plus flexible sigmoidoscopy -- though virtual colonoscopy may have benefits for screening laggards -- according to a new model analysis in Radiology.
Using data from the National CT Colonography Trial (NCTCT), the authors found that in general, colonoscopy, fecal immunochemical test (FIT) plus flexible sigmoidoscopy, and fecal occult blood test (FOBT) plus flexible sigmoidoscopy all increased life expectancy and reduced lifetime risk of colorectal cancer more than screening every five or 10 years with virtual colonoscopy (also known at CT colonography or CTC).
In direct comparison, conventional colonoscopy was more cost-effective than virtual colonoscopy in most scenarios, the authors found. When screening compliance was reduced to 50%, however, CTC came out ahead in two of the three simulation models used in the analysis.
There were questions about the study's methodology from a CTC practitioner, who said that the model's 95% completion rate for optical colonoscopy seemed unrealistically high; that VC's true cost was probably lower than that of conventional colonoscopy, thereby skewing the model; and that the study didn't consider the high percentage of individuals who refuse to undergo other colon cancer screening tests.
"I think the results suggest that virtual colonoscopy has a role for people who are unwilling or unable to undergo other screening tests, and if there's a segment of the population that is willing to try VC but not the others, my personal opinion is that this paper encourages them to do so because [VC] is clearly better than not screening," responded lead author David Vanness, PhD, in an interview with AuntMinnie.com. Vanness is an assistant professor of population health sciences at the University of Wisconsin School of Medicine.
Based on results of multicenter CTC trial
The 2008 NCTCT trial -- to date, the largest multicenter study to assess CTC's effectiveness -- was designed to address widely varying results from previously conducted CT colonography trials. Results of the NCTCT confirmed that CT colonography depicts colorectal adenomas and carcinomas (neoplasia) with sensitivities of 78% to 90% and specificities of 86% to 88%, depending on lesion size (New England Journal of Medicine, September 18, 2008, Vol. 359:12, pp. 1208-1217).
"It remains unclear whether, given these performance characteristics, screening with CT colonography is an efficient use of resources," wrote Vanness, Amy Knudsen, PhD, and colleagues (Radiology, August 3, 2011).
Joint guidelines from the American Cancer Society and the U.S. Multisociety Task Force on Colorectal Cancer recommend various options for screening average-risk individuals ages 50 years and older for colorectal cancer (CRC), including CTC every five years. However, the U.S. Preventive Services Task Force excludes CT colonography from its guidelines due to a 2008 opinion that there was insufficient evidence to recommend it for widespread screening.
The study's estimates of CTC performance from the NCTCT trial were incorporated into three previously validated Cancer Intervention and Surveillance Modeling Network (CISNET) CRC microsimulations: MISCAN-COLON, CRC-SPIN, and SimCRC. Each model uses common data and a unique model structure to simulate the natural history of CRC. The aim of the study was to estimate the cost-effectiveness of CT colonography for CRC screening in average-risk 50-year-old asymptomatic subjects.
Analyses of survival and lifetime costs for screening with CTC every five or 10 years were compared with conventional colonoscopy, flexible sigmoidoscopy plus either sensitive unrehydrated FOBT or FIT, and no screening based on the three models.
The researchers modeled perfect screening compliance, as well as reduced adherence (showing up for screening half as often as recommended, but always proceeding to colonoscopy if the test result was positive). They calculated both the incremental cost-effectiveness and estimated net health benefits from the U.S. provider perspective. Data regarding natural history and non-CRC deaths were gleaned from Surveillance, Epidemiology, and End Results (SEER) data from 1996 to 1999.
Medicare data (2007) were used to estimate screening costs. Because the U.S. Centers for Medicare and Medicaid Services has not assigned relative value units for screening CTC, however, the authors were left to estimate CTC costs by summing reimbursement-based cost estimates for noncontrast CT of the abdomen and pelvis, noncontrast pelvis, and 3D reconstruction, adjusted for resource savings associated with imaging contiguous anatomic regions.
Next, incremental cost-effectiveness ratios (ICERs) were calculated for each strategy as a ratio of the incremental cost versus life-years gained, compared with the next least-costly screening strategy.
Effective but costlier than stool tests
At 100% screening adherence, all three models found that colonoscopy, FIT plus flexible sigmoidoscopy, and FOBT plus flexible sigmoidoscopy all increased life expectancy and reduced lifetime CRC risk more than CT colonographic screening at five- or 10-year intervals.
However, when screening compliance was reduced to 50%, performing CT colonography every five years reduced the risk of colon cancer more than colonoscopy did in two of the three models (MISCAN: 39.1% versus 38.7%; SimCRC: 61.6% versus 59.5%). CTC also had higher undiscounted life-years gained than colonoscopy in all models, Vanness and colleagues wrote.
"CT colonography at five- and 10-year screening intervals was more costly and less effective than FOBT plus flexible sigmoidoscopy in all three models in both 100% and 50% adherence scenarios," they wrote. Colonoscopy also was more costly and less effective than FOBT plus flexible sigmoidoscopy, except in the CRC-SPIN model assuming 100% adherence (ICER: $26,300 per life-year gained).
CT colonography at five- and 10-year screening intervals and colonoscopy were beneficial compared with no screening in each of the model scenarios. CTC at a five-year screening interval was more beneficial than the 10-year interval except in the MISCAN model at 100% adherence, and assuming a willingness to pay $50,000 per life-year gained, the authors wrote.
"All models found that CT colonography at either five- or 10-year intervals is likely to be cost-effective relative to no screening, but both strategies were dominated by conventional screening tests," Vanness and colleagues wrote. "The models also found colonoscopy likely to be more costly and less effective than FOBT plus flexible sigmoidoscopy (except with perfect adherence in one model), yet colonoscopy is likely to be net beneficial compared with no screening."
The results confirm those of previous Markov models finding virtual colonoscopy at five-or 10-year intervals to be cost-effective compared with no screening ($4,400-$28,700 per life-year gained) but not cost-effective compared with colonoscopy, they wrote. However, the new multimodel approach is an improvement because it allows "investigation of convergent validity -- the extent to which results are sensitive to model specification."
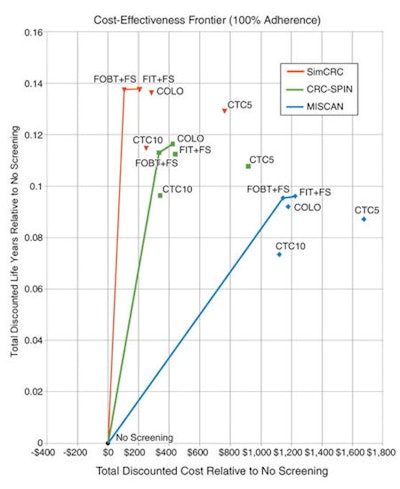 |
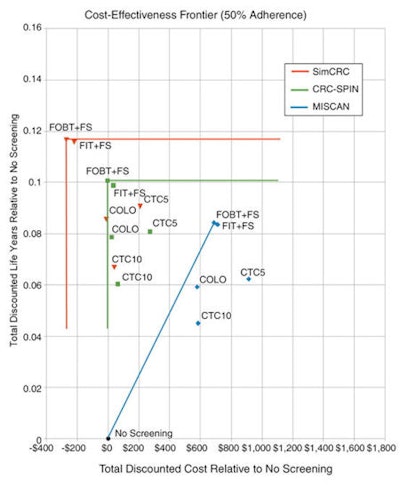
| The results demonstrate that FOBT plus flexible sigmoidoscopy, FIT plus flexible sigmoidoscopy, and colonoscopy are generally more economically efficient than CTC at five- or 10-year intervals; however, with 50% screening adherence, SimCRC found CTC every five years to be more economically efficient than colonoscopy at all three opportunity costs. These charts depict a frontier analysis of cost-effectiveness at 100% patient compliance (above) and 50% compliance (below). Strategies lying below and to the right of the frontier are either dominated (more costly and less effective than a specific alternative strategy) or extended-dominated (more costly and less effective than a linear combination of two strategies). Strategies on the frontier represent an efficient use of resources for some willingness to pay per life-year gained. COLO = colonoscopy at 10-year intervals; CTC5 = CTC with 5-mm referral threshold at five-year intervals; CTC10 = CTC with 5-mm referral threshold at 10-year intervals; FIT + FS = annual FIT plus flexible sigmoidoscopy at five-year intervals; FOBT + FS = annual unrehydrated FOBT plus flexible sigmoidoscopy at five-year intervals. Images republished with permission of the RSNA from Radiology, August 3, 2011. |
 |
As for limitations, the authors noted that extracolonic findings were unaccounted for in the study, and they may have over- or underestimated compliance rates for the probability that some tests are more attractive than others. Nor did the model address the value of other screening exams, such as for abdominal aortic aneurysm (AAA) or bone mineral density assessment, that can be performed using CTC data. In addition, Medicare cost data may not accurately account for higher costs associated with novel chemotherapeutics and biologics, and not all individuals with a positive FOBT test will proceed to colonoscopy, as the study assumes. Finally, the authors did not account for quality of life.
For an asymptomatic, average-risk screening cohort, CTC every five or 10 years is more costly and less effective than non-CTC approaches at five or 10 years, the group concluded. Still, CTC was probably beneficial compared to no screening, and five-year screening intervals are probably more beneficial than 10-year intervals, they added. "That three independent models reached similar conclusions adds credibility to our findings," Vanness and colleagues wrote.
Input data questioned
"My personal experience and that of many of my colleagues suggest a few critical input parameters that could drastically alter the results in favor of CTC," wrote Dr. Abraham Dachman, professor of radiology and head of CT imaging at the University of Chicago, in an email to AuntMinnie.com. First, he said, colonoscopy completion rates can vary widely in practice and are documented at 2% to 10% in the gastroenterology literature.
Vanness said the 5% rate used in the model was fair, since it represented the higher of two failure rates from Sinaka et al, who in 2006 compared morning (3.2% failure) and afternoon (5.2% failure) colonoscopy results in more than 2,000 colonoscopies (American Journal of Gastroenterology, December 2006, Vol. 101:12, pp. 2726-2730). Vanness acknowledged that failure rates can be higher in daily clinical practice, which would have the effect of raising the comparative costs of conventional colonoscopy.
Dachman also said that billed charges for virtual colonoscopy in practice tend to be lower than for conventional colonoscopy, which, if true, would also make the virtual exam more favorable.
"I've found many places that charge 50% or less for CTC versus [optical colonoscopy] -- so each institution needs to look at their own cost ratio before assuming these results apply to them," Dachman wrote.
But Vanness countered that billed charges bear little relation to money actually collected, and because true Medicare charges don't yet exist, resource-based relative value scale (RBRVS) estimates continue to be a good choice for estimating costs.
"That's why we used RBRVS, even though it has its own methodological problems -- because it is the basis of a large portion of payments, and it's supposed to be resource-based," Vanness said. The drawback of modeling is that it depends on numerous assumptions, and the sensitivity to key inputs is not characterized, he wrote. So while they are useful for individual decision-making, models have doubtful population validity, and as the population characteristics change, so do the results. "We were as accurate as we could be in reflecting what the trial told us using the best models available," Vanness said.
"We did a lot of sensitivity analyses to determine how cheap VC had to be relative to [optical colonoscopy] in order to be considered the best test overall," and left it up to the reader to determine if those costs made VC a good deal, he said. On the other hand, "VC would have to be extremely expensive not to be worthwhile at all," Vanness said.
Dachman called CTC a valuable addition to colorectal cancer screening at the University of Chicago, one that could help coax the 40% of the eligible population who are unscreened to get screened, if it's made universally available.
"Even highly educated patients may have other reasons for opting for CTC as did President Obama," Dachman said. "If we knew the number of patients who would undergo CTC but refuse initial screening with [optical colonoscopy], the cost-effectiveness of CTC would also improve dramatically."




















