Dear CT Insider,
A new era in targeted cancer therapies requires new approaches to measuring treatment response. As a result, researchers are constantly on the hunt for biomarkers more nuanced than tumor size to evaluate the effectiveness of those therapies.
CT perfusion is a promising way to gauge treatment response, for example, but some centers find it a little too complex and exacting for routine clinical use. A simpler approach involves updating an old technique to make it new again -- like evaluating contrast uptake quantitatively.
Researchers from Massachusetts General Hospital are proposing non-necrotic tumor volume measurement to determine viable tumor size following therapy for hepatocellular carcinoma. In a pilot study, their technique outperformed total tumor volume and the latest Response Evaluation Criteria In Solid Tumors (RECIST) techniques in predicting survival. Get the details by clicking here.
The Joint Commission's new foray into the imaging accreditation business is also shaking things up, though the American College of Radiology says it's not worried about the competition, in a story you'll find here.
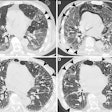
In chest imaging news, you know all those lung nodule follow-ups recommended in the Fleischner Society guidelines? They can be performed at super-low doses, say researchers who looked into the matter. And a new article in the Journal of the American College of Radiology offers easy-to-follow tips for keeping chest CT doses low.
In interventional radiology, learn how researchers in China are halving the dose by eliminating redundancies.
In cardiac imaging, a new technique to measure fractional flow reserve moves CT another step forward in becoming a one-stop shop for gauging heart function and coronary artery patency in a single exam.
Just scroll down through the links below for more news you don't want to miss -- all in your CT Digital Community.