
The scan radiologists love to hate can be a lifesaver. Yet most CT pulmonary angiography (CTPA) scans for suspected pulmonary embolism (PE) come up negative, even in the population that might be expected to have the greatest risk: patients presenting to the emergency department with symptoms suggestive of PE.
Still, nearly a third of all patients presenting to the emergency department at Rossi University Hospital in Verona, Italy, came up positive for pulmonary embolism, a little higher than expected.
The study also found deep vein thrombosis (DVT) in about 10% of patients, along with high correlation of MDCT with D-dimer results. But adding CT venography to look for DVT in the abdomen and pelvis is a bad deal, investigators said.
The CTPA study came from "our desire to review the prevalence of CTPA in patients with a clinical suspicion of acute PE over a 12-month period," said Dr. Giulia Zamboni in a presentation at the 2012 European Congress of Radiology (ECR). "We also wanted to assess the diagnosis and presence of unexpected findings, which is not uncommon in patients with suspected acute PE."
The primary goal was to assess PE prevalence in the patients presenting to the emergency department with suspected acute PE, as well as collateral findings of the chest, she said. The secondary goal was to evaluate the results of a venous scan of the abdomen and pelvis following completion of CTPA. Finally, the group also looked at the diagnostic results of D-dimer assay as a predictor of PE.
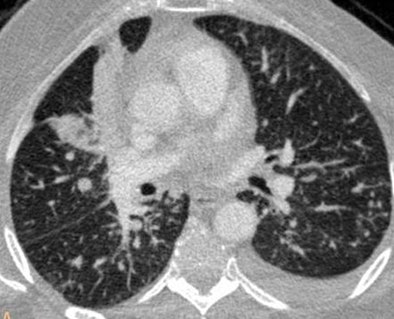
 |
| Axial image shows extensive filling defects in the pulmonary trunk and the main pulmonary arteries. A solid lesion is seen in the left lung. Bilateral pleural effusion is also present. All images courtesy of Dr. Giulia Zamboni. |
The study population included 239 patients (111 men, 128 women; mean age, 67.1 years) including 92 who presented to the emergency department and another 147 inpatients at the hospital during 2010, Zamboni said.
Using a 64-detector-row scanner, the researchers evaluated 201 patients with a standard 120-kV protocol and 38 with a low-dose 80-kV protocol, following injection of 1.5-mL/cm/kg contrast media at a minimum of 4 mL per sec.
PE was categorized as massive (affecting the main trunk) or nonmassive (segmental or subsegmental emboli), and the study team logged the prevalence of other chest findings such as pulmonary consolidation, pleural effusion and atelectasis, and tumors, primary or secondary. A venous scan of the abdomen and pelvis was added to look for DVT, and correlation between D-dimer levels and PE was calculated.
 |
| Sagittal image shows a massive filling defect in the pulmonary trunk. Multiple vertebral and sternal fractures are also depicted. |
The results showed PE in 73 (30.5%) of 239 patients; of these cases, 45 (61.6%) were categorized as massive and 28 (38.4%) as nonmassive.
Collateral findings in patients with PE included pleural effusion (n = 27), parenchymal consolidation (n = 15), and tumors (n = 7). In 165 scans that were negative for PE, 75 patients had no significant findings at CT and 90 had pleural effusion (n = 66), parenchymal consolidation (n = 36), or tumors (n = 10).
One hundred sixty of these 165 patients had D-dimer levels greater than 500 ng/dL, which yielded sensitivity of 100%, specificity of 3.9%, positive predictive value of 33.1%, and negative predictive value of 100%.
 |
| Axial image shows an area of consolidation in the middle lobe, multiple bilateral small nodules, and left pleural effusion. No filling defects are seen in the pulmonary arteries. |
"It's not surprising that D-dimer has a very high sensitivity but low specificity," she said. And the 30% prevalence of PE was higher than expected.
"The most common collateral finding was the presence of pleural effusion with atelectasis -- less common were consolidation and tumors," Zamboni said. Fourteen percent of all patients scanned in the abdomen and pelvis had DVT somewhere in this region.
"But where was this DVT? If we break up the results, we find that nearly half of our cases of DVT were in the femoral veins," Zamboni said. "Only a little more than half were in the inferior vena cava or iliac veins, which might be a little more difficult to explore with ultrasound."
The mean radiation dose delivered by the scans was slightly greater than 7 mSv, Zamboni said.
"Even in a population with a prevalence of PE that is similar to or slightly higher than what is reported in the literature, most of the exams we are going to perform will not have PE -- but MDCT allows us to have a concurrent or alternative diagnosis," she said.
The low prevalence of DVT among patients scanned in the abdomen and pelvis shows that "the extra radiation we administer to these patients is not justified, especially if we consider that nearly half the cases of DVT that we saw were in the femoral veins, which we can very nicely explore with ultrasound," Zamboni said.




















