
A new dual-energy CT angiography (DECTA) protocol may provide a more accurate look at coronary artery calcium by eliminating artifacts that can bedevil more conventional CTA approaches, according to researchers from Virginia at this week's Society of Cardiovascular Computed Tomography (SCCT) meeting in Baltimore.
In a study billed as the first to scan human subjects with DECTA along with conventional CT angiography and in some cases conventional angiography, researchers found that calcified plaques were about one-fifth smaller on DECTA. The dual-energy technique also depicted the vessel lumen as about one-fourth larger than on conventional CT images.
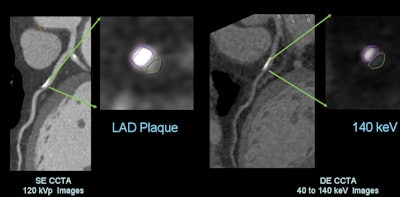 |
| Use of monochromatic imaging at coronary CTA reduces the size of calcified plaques and increases lumen size compared to conventional single-energy CT. All images courtesy of Dr. James Earls. |
The technology could reduce downstream testing by giving physicians a better look at lumen morphology and potentially reducing false positives, said lead researcher Dr. James Earls in an interview with AuntMinnie.com.
"Hopefully, it will more accurately characterize people's disease, and since you'll have fewer false positives, people won't be going on for additional testing and they'll just be medically managed," said Earls, a radiologist with Fairfax Radiology Associates.
His research colleagues included Dr. Jonathon Leipsic and Dr. Brett Heilbron from the University of British Columbia; Dr. David Dowe from Atlantic Medical Imaging in Galloway, NJ; Dr. Sachio Kuribayashi from Keio University in Japan; and Dr. James Min from Cedars-Sinai Medical Center.
The presence of calcified arterial plaque has always been a problem on coronary CTA because it leads to overestimation of coronary stenosis and false-positive findings, Earls said.
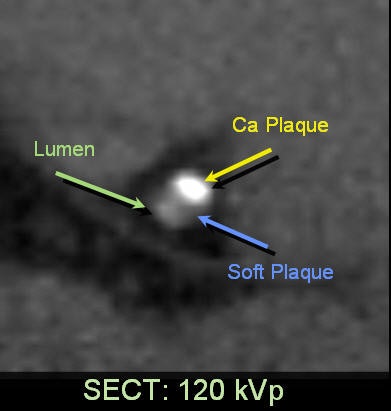
Plaque appears larger than life on conventional CTA due to several factors, including beam hardening, aliasing, scatter, partial-volume effects, and edge-gradient artifacts, which decrease positive predictive value due to false positives, he said. The effect is well-known thanks to studies that have compared conventional CT with invasive angiography.
A paper by Voros et al in 2011, for example, showed that calcium blooming at CT increases calcified plaque volume by 104%, reduces luminal diameter by 21%, and increases perceived stenosis diameter by 39% compared to conventional angiography.
Earls and colleagues hypothesized that projection-based dual-energy CT might reduce these artifacts, displaying a more accurate representation of plaque and improving overall diagnostic performance. They aimed to perform the first human assessment evaluating the effects of monochromatic single-energy projection-based DECT with single-energy CT and conventional angiography.
A dual-energy CT scanner (Discovery CT750 HD, GE Healthcare) with the Gemstone Spectral Imaging (GSI) Cardiac package was used for the study. Earls and colleagues scanned patients using a prospective electrocardiogram triggering protocol (64 x 0.625 mm), rapid 0.5-msec switching between 80 and 140 kV, iterative reconstruction (adaptive statistical iterative reconstruction), and available monochromatic and material composition imaging.
The two energies are used to create interleaved high and low kVp projections, which are then reconstructed into images that allow for registered spectral CT images. In the study, attenuation-to-material density transformation separating iodine and water were used to create monochromatic images in 10-keV increments from 40 to 140 keV.
The prospective study examined 39 patients (mean age, 57.5 ± 12.2 years; mean body mass index, 27.41 ± 4.39), who signed written disclosures before undergoing two CT scans each: dual-energy rapid-kVp-switching prospectively triggered coronary CTA, and traditional single-source coronary CTA.
Thirty coronary plaques (10 calcified, 10 mixed, and 10 soft plaques) were chosen for analysis. The readers measured lumen area adjacent to the plaque at the area of maximal stenosis, as well as plaque area, lumen diameter, and vessel diameter. The median effective radiation dose was 3.8 ± 1.2 mSv, compared with 3.1 ± 1.1 mSv for single-source CT, a difference that did not reach statistical significance.
The percentage stenosis decreased with increasing monochromatic energy levels. Plaques were largest at 40 keV and smallest at 140 keV, with little change at 100 keV and greater. In nine of 10 cases, high-keV monochromatic images had substantially less lumen reduction at 140 kVp compared to 120 kVp.
"As we increase the energy, the blooming artifact gets smaller and smaller and smaller, and by the time we get up to 140 keV we may be approaching a much more true representation of how big the calcified plaque is," Earls explained. "The really big difference was from 40 to 80 keV where it got dramatically smaller, then from 80 up to 140 keV it really didn't change that much."
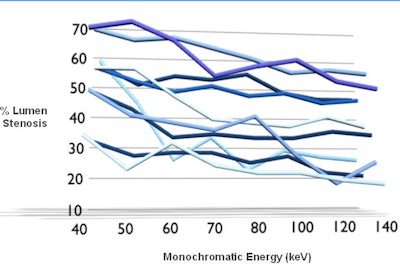 |
| The percentage stenosis decreased with increasing monochromatic energy. Plaques were largest at 40 keV and smallest at 140 keV, with little change at 100 keV and greater. |
Compared to single-source CT, the 140-keV monochromatic images at DECT showed 21.3% ± 11.3% greater arterial lumen area and 11.3% ± 7.3% greater luminal diameter. The calcified plaque area decreased by 26.4% ± 10.8% and plaque diameter decreased 15.2% ± 9.3% (p < 0.05), Earls said.
For mixed plaques, DECT 140-keV monochromatic images showed greater arterial lumen area of 10.4% ± 8.8% and greater luminal diameter of 5.7% ± 7.0%. Plaque area decreased 17.4% ± 11.3% and plaque diameter decreased 11.2% ± 5.2% (p > 0.05) compared to single-source CT. For soft plaques, the size change was negligible, Earls said.
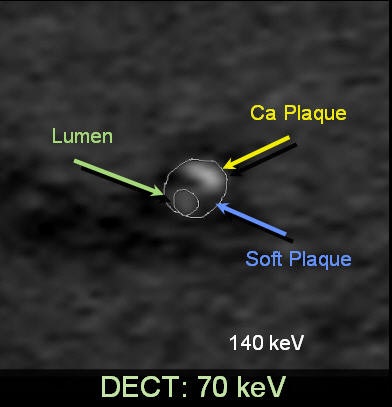 |
| Mixed plaque image at DECT (above) shows smaller volume of calcified plaque compared to single-source CT from the same coronary artery segment (below). |
 |
Compared with conventional angiography, the diameter reduction shown at 140-keV DECT was closer than that of single-source CT images in six of six (100%) calcified plaques, three of four (75%) mixed plaques, and two of four (50%) soft plaques, the group reported in an accompanying abstract.
"The percentage stenosis was 25% less on the dual-energy CT than it was on single-energy CT," Earls said. One can imagine a situation "where conventional CT was showing an 80% or 90% stenosis, but then you do a DECT and it shows only a 60% stenosis. That might actually end up changing management of the patient; maybe the patient doesn't have to go on to a cardiac catheterization, whereas they would have by relying on the conventional CT."
Compared to single-energy CT, projection-based DECT provides a significant reduction in artifact from calcified and mixed coronary plaques and depicts stenoses that more closely represent those found at conventional angiography, he said.
The dual-energy CTA technique the researchers used is feasible to perform, and the radiation dose isn't significantly higher compared to single-source CT, Earls said. The greatest effect of DECT is seen in higher-keV (100 to 140) images.
"Every once in a while in CT we get these jumps in technology that really can help us," Earls said. "We've all struggled with the calcium issue for years, and this is the first thing I've seen that has truly looked like it's going to minimize some of the artifacts that we haven't been able to do anything about in the past."
The technology should improve the specificity of cardiac CTA, which in many cases will be the only test that the patient needs, potentially eliminating many catheterization procedures and SPECT exams, he said.
"The people I'm going to use this on are people I suspect have a lot of atherosclerosis," he said. "If I suspect they're not going to have a lot of disease, or on their scout views I don't see any calcium, then I will probably use the conventional [single-energy CT] technique."
|
Study disclosures Earls receives consulting fees from GE Healthcare. Min has served on the speaker's bureau and on the medical advisory board of GE. Dowe is a consultant for GE and is on the speaker's bureau. Leipsic is a member of the speaker's bureau and has served as a consultant to GE. |




















