Coronary CT angiography (CCTA) was nearly perfectly in line with cardiac catheterization in its selection of therapies for patients with a high likelihood of coronary artery disease (CAD), according to a new study in Radiology. The results showed that CCTA can determine patient management as well as invasive angiography while sparing many patients from invasive procedures, researchers said.
In a study of patients with a positive SPECT myocardial perfusion imaging (MPI) studies, CCTA results pointed to the same therapeutic strategy as invasive coronary angiography -- intervention versus conservative care -- nearly 100% of the time, while also picking the choice of therapy in patients who needed revascularization -- percutaneous coronary intervention (PCI) versus coronary artery bypass grafting (CABG) -- in more than 90% of cases.
The study found that CCTA demonstrates equivalent accuracy with angiography in differentiating the need for revascularization, and even the type of revascularization in patients with suspected coronary artery disease and a positive SPECT exam, wrote Dr. Antonio Moscariello and colleagues from the Medical University of South Carolina (Radiology, August 8, 2012).
"Coronary CT angiography has the potential to act as an effective secondary gatekeeper after a positive nuclear myocardial perfusion study, limiting the number of patients without obstructive CAD who undergo conventional cardiac catheterization and informing decision making with regard to revascularization," they wrote.
Little info on CCTA guiding care
Ample evidence in the literature supports the use of CCTA for ruling out coronary artery disease, but surprisingly little information is available about the role of coronary CT angiography in guiding patient care beyond its ability to exclude significant stenosis, Moscariello wrote.
"The number of cardiac catheterizations that are not followed by an interventional procedure is substantial and improvements in the strategies for decision-making regarding revascularization are desirable," they wrote.
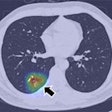
Moscariello and colleagues, including Drs. Rozemarijn Vliegenthart, U. Joseph Schoepf, and John Nance, looked at 185 consecutive patients (121 men, 64 women; mean age 59.4 years ± 9.7) with a positive SPECT MPI study demonstrating a stress score of 9 or greater within the previous month. The patients had presented with nonacute chest pain (stable angina or atypical chest pain) who had been referred for elective conventional cardiac catheterization. Patients were excluded if they needed urgent cardiac catheterization, had a history of CAD, or general contraindications to CT angiography.
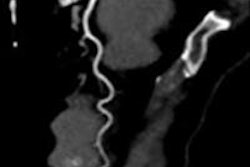
Up to a week before catheterization, patients underwent dual-source CT (Somatom Definition or Definition Flash, Siemens Healthcare) using a technique selected for each patient depending on heart rate and rhythm, as well as body mass index (BMI). ECG-triggered tube current modulation and prospective triggering were used by default, and either 100 kV or 120 kV depending on BMI. Patients received sublingual nitroglycerin and beta-blockers in addition to iodinated contrast before the scans. Two experienced readers examined the data jointly on a workstation using the American Heart Association's 15-segment model.
Among the 185 patients undergoing CCTA, 67 had retrospectively ECG-gated CCTA (mean radiation dose of 10.3 mSv), 104 underwent prospectively ECG-triggered CCTA (mean dose of 6.1 mSv), and 14 underwent prospectively ECG-triggered high-pitch spiral CCTA (mean dose of 2.1 mSv), at a mean heart rate of 65 beats per minute (bpm).
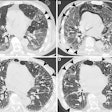
Cardiac catheterization revealed obstructive lesions in 75 (41%) patients and 287 (10%) segments. In all, 110 of the 185 patients either had normal coronary arteries (n = 42, 23%) or nonsignificant lesions with less than 50% luminal narrowing (n = 68, 37%), Moscariello and colleagues wrote.
In 96% of patients (n = 178), CCTA and coronary catheterization identified the same therapeutic strategy in terms of conservative treatment versus revascularization, and all patients in need of revascularization were identified with coronary CT angiography, the study team reported. When revascularization was indicated, both exams chose the same procedure (PCI or CABG) in 92% (n = 66) patients.
Performance of CCTA vs. angiography for treatment strategy
|
In this group of patients with a positive SPECT exam, decisions made on the basis of CCTA results were similar to those made with cardiac cath, Moscariello and colleagues wrote.
"Coronary CT angiography has the potential to act as an effective secondary gatekeeper after a positive nuclear myocardial perfusion study, limiting the number of patients without obstructive CAD who undergo conventional cardiac catheterization and informing decision-making with regard to revascularization," they concluded.
The study population closely mirrors real-world statistics with regard to patients undergoing elective coronary catheterization in the U.S., except for a preponderance of male patients due to some patient recruitment from U.S. Department of Veterans Affairs hospitals, they noted.
Not only did CCTA identify all patients in need of revascularization, there were only seven false-positives who did not need revascularization after angiography, Moscariello and colleagues wrote.
"These findings indicate the strong potential for reducing unnecessary diagnostic catheterization procedures if coronary CT angiography is integrated into the diagnostic algorithm of suspected CAD," and of informing decision-making regarding the need for revascularization, they wrote.