In a comparison of patients with ischemia detected by SPECT or PET myocardial perfusion imaging (MPI), resting electrocardiogram-gated 64-slice MDCT proved "unsuitable" for clinical use, according to a study published in the February issue of the American Journal of Roentgenology.
Researchers from Montefiore Medical Center found that MDCT consistently achieved less sensitivity and specificity than the other two modalities in a visual analysis of imaging results of 580 myocardial segments.
As lead study author Dr. Ari Spiro, from the department of radiology at Albert Einstein College of Medicine, and colleagues noted, myocardial ischemia is an important indicator for patient outcome in the management of coronary artery disease (CAD), with radionuclide MPI as the method of choice to assess ischemia.
While MDCT during stress has been explored for myocardial perfusion, "there is a paucity of literature dedicated to evaluating the myocardium at rest," the authors wrote (AJR, February 2013, Vol. 200:2, pp. 337-342).
Spiro and colleagues retrospectively identified patients who underwent stress radionuclide SPECT or PET MPI at Montefiore between January 2006 and October 2009. The same patients also underwent retrospectively gated cardiac CT within 90 days of MPI.
The study culled its cohort into a group of 20 women and 15 men, who had a mean age of 52 years (range, 17 to 74 years). All 35 individuals had ischemic myocardial perfusion on SPECT or PET and had archived images of left ventricular CT during both systole and diastole.
Stress tests were conducted either on a treadmill using the Bruce protocol or via four-minute adenosine protocols with or without the use of low-level treadmill exercise. SPECT images were acquired using a dual-headed gamma camera (Vertex, Philips Healthcare).
The majority of patients underwent one-day dual-isotope MPI with 3 mCi (110 MBq) of thallium-201 chloride for rest and 30 mCi (1,100 MBq) of technetium-99m sestamibi for the stress test. Coronary CT angiography was performed using a 64-slice MDCT scanner (LightSpeed VCT, GE Healthcare).
Spiro and colleagues used both visual means and an automated method to measure myocardial perfusion on MDCT. The visual technique retrospectively evaluated systole and diastole data for all 35 patients; adequate data were available for the automated analysis for 34 patients.
The group then calculated sensitivity, specificity, positive predictive value, and negative predictive value for the visual method in systole and diastole, using MPI as the standard of reference.
Visual analysis
A total of 595 segments were visualized on MPI. There were 152 ischemic segments and 428 nonischemic segments among the 35 subjects; 15 segments were excluded due to the presence of fatty replacement on CT.
In the visual analysis for MDCT perfusion in systole, sensitivity was low at 16%, having discovered only 24 of the 152 ischemic segments seen by MPI. MDCT detected 393 of 428 nonischemic segments, for a specificity of 92%. MDCT had a positive predictive value of 40% and negative predictive value of 75%.
In diastole, MDCT achieved sensitivity of 18% (27 of 152 ischemic segments), and specificity reached 89% (382 of 428 nonischemic segments). Positive predictive value was 37%, while negative predictive value was 75%.
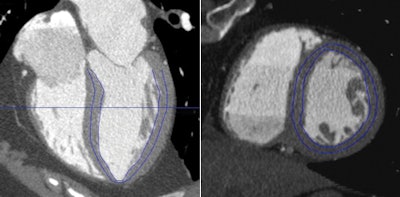 |
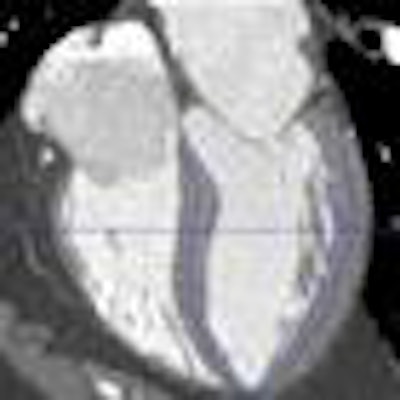
| Images are from a 60-year-old woman with obstructive coronary artery disease in the left anterior descending and left circumflex territories. A time-volume analysis tool was used to evaluate subendocardial attenuation. Automated left ventricular wall segmentation is adjusted manually to select subendocardium (blue outline), as shown in horizontal long-axis (left) and short-axis (right) views. Images courtesy of AJR. |
In other findings, there was no significant difference in CT perfusion between patients with and without obstructive CAD on CT angiography using the visual or automated methods.
CT angiography showed that 20 individuals (57%) had no evidence of obstructive CAD with the visual analysis, while 15 (43%) had obstructive CAD. The automated visualization method had essentially identical results, finding 14 cases of obstructive CAD and 20 individuals with no obstructive CAD.
"Although different attenuations were subjectively detected on visual inspection of some segments, the performance characteristics of visual analysis [of MDCT] were not suitable for clinical diagnosis," Spiro and colleagues concluded.
Given that MDCT underperformed in patients with obstructive CAD on CT angiography, "visual analysis of resting CT datasets for perfusion abnormalities in areas of myocardium subtended by stenosed vessels may also be inaccurate," they wrote.