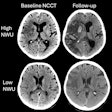
"If you see a small core and an M1 occlusion, you're probably going to want to bring that patient to treatment, and there's probably nothing else you need to know in terms of both safety and efficacy," he said. "We looked at a series of these ... for a pilot study back in 2009, and it showed that CT perfusion and MR perfusion weren't adding useful clinical information. But they did show something more interesting and important about the role of imaging."
Yoo et al (Stroke, 2009, Vol. 40, pp. 2046-2054) showed that patients with more than 70 mL of lesion volume at admission had poor clinical outcomes regardless of other variables, rendering the DWI protocol "futile," Lev said. "If anything they were at increased risk of hemorrhage if you treated them. We didn't know that when we did the study and we did treat a lot of patients with small DWI [lesions], and for a lot of these DWIs it didn't matter."
However, "if there was no recanalization, even patients with small initial DWIs did poorly," he said. So patients with large DWI lesions at admission or M1 occlusion with no recanalization had poor outcomes, but patients with both early and late recanalization did well, and the earlier the recanalization, the better the outcome.
Sixty-four percent of patients with early recanalization of small DWI lesions had good outcomes, versus just 15% of those with late recanalization, he said. But the most interesting thing about the study by Yoo et al was how early and late recanalization were defined: not from the length of time between stroke onset and treatment, but from the time of diffusion imaging to treatment, Lev said.
Imaging is brain
"What does this mean? When we stratified time post-ictus there was no relationship, but when we stratified time post-DWI we had this relationship" between time delay and outcomes, Lev said. "So from the time of imaging, if you see a favorable imaging profile for treatment, you should treat the patient, and it almost doesn't matter what the clock is telling you, it only matters what the images are telling you. If there's a small lesion and an M1 occlusion, you should treat that patient. And the sooner you treat the patient, the more likely they will do well."
Thus, the infarct core measurement is critical, and Yoo et al also showed that the adage "time is brain" should be replaced with "imaging is brain" for patient selection, Lev said.
At Lev's center, the imaging algorithm for determining the need for endovascular therapy calls for unenhanced CT and always a CTA exam, which doesn't require extra time because it can be performed during the 10 minutes that the IV-tPA is being mixed, Lev said. A DWI scan for other reasons never hurts if one can be performed, "but we won't let the perfusion imaging slow us down if we're taking the patient to endovascular therapy," he said.
"Where to start the clock is a major question due to enormous variability in the rate at which neurons die, and the trouble with imaging is that it's just a snapshot in time," he said. "In most patients without recanalization a large perfusion deficit at admission is tied to a large DWI lesion at admission, even though the tests measure different things, so it's impossible to know for sure if the two factors will be correlated."
Research continues, and the findings to date aren't absolute. If a patient with a large cholinergic basal forebrain lesion were treated within 90 minutes, it could be reversible, and a different combination of parameters -- for example, fluid-attenuated inversion recovery (FLAIR)-DWI mismatch -- is being looked at to answer this question, Lev said. Clinical trials are now testing late IV thrombolysis in stroke of unknown onset time based only on FLAIR onset to DWI.
FLAIR MRI takes six hours (plus or minus five) to become positive after stroke, he said, while DWI becomes positive in 30 to 90 minutes, "so if there's a big DWI lesion but a small FLAIR lesion, it might be safe to treat that patient," he said. "That's another thing being looked at with DWI as the gold standard, but in the absence of DWI images comparing CTA to CTA [source images] hasn't worked out well."
The group also continues its research into collateral vessels, which can supply tissues surrounding an infarct with blood and reduce brain loss. A lack of collateral vessels -- a collateral score of 0 -- is associated with "malignant pattern" or poor outcome, even when early intervention or small infarct size might portend more favorable results, Lev said.
In summary, even if perfusion CT doesn't inform the treatment decision, it is useful for many diagnostic tasks including infarct detection, differential diagnosis, transient ischemic attack assessment, vasospasm, intensive care unit monitoring, and hypertension, Lev said.
"There are all kinds of reasons to get perfusion, but for thrombolysis treatment itself? That's probably not one of them," he said.
Previous page | 2