Functional MRI (fMRI) has found a strong association between depression in stroke patients and functional impairment when the brain is in a resting state, according to a study published online June 5 in Radiology. The discovery could lead to better treatment for these individuals.
The findings support the theory that impairment of brain function is more important in assessing poststroke depression than finding damage to structural areas such as lesions. The study may help the clinical management of stroke patients by providing an opportunity to investigate the effects of a variety of treatments, according to lead researcher Dr. Igor Sibon, PhD, professor of neurology at the University of Bordeaux, and colleagues.
Approximately one-third of patients who survive a stroke experience poststroke depression, Sibon and colleagues noted. Previous studies, however, have yet to identify a link between brain lesions caused by ischemia during a stroke and subsequent depression.
Default mode network
Rather than look for abnormalities and dysfunction in specific regions of the brain after stroke, the researchers chose to look for impairment in brain function. They evaluated a group of brain structures in the default mode network, a resting-state neural network that is active when an individual is not focused on external tasks. Changes in conductivity in the default mode network have been seen in patients with depression.
The prospective study enrolled 32 consecutive patients between the ages of 18 and 80 years from September 2000 to October 2008, during which time the individuals experienced their first mild to moderate ischemic stroke.
The researchers excluded patients with aphasia; a history of psychiatric or neurologic disorder; or a history of lesions affecting one structure of the default mode network, which includes the medial prefrontal cortex and the anterior cingulate cortex.
Patients were clinically evaluated between six and 14 days after the stroke and again between 2.5 and 3.5 months afterward, with two of the study authors performing the clinical evaluations. A diagnosis of poststroke depression was made three months after stroke.
Stroke severity was based on the U.S. National Institutes of Health's Stroke Severity scores and other rating scales. The severity of depression and anxiety symptoms were measured through the Hamilton Depression Rating Scale 17 (HDRS 17) and the Hamilton Anxiety Rating Scale (HARS) 10 days and three months after stroke.
MRI protocol
MRI scans were performed 10 days after the stroke using a 1.5-tesla scanner (Intera, Philips Healthcare) and a phased-array sensitivity-encoding head coil. The researchers used fluid-attenuated inversion recovery (FLAIR) diffusion- and perfusion-weighted MR images to characterize cerebrovascular lesions. In addition, resting-state fMRI was utilized to determine functional connectivity in the default mode network, and T1-weighted 3D images were acquired to localize functional data.
A total of 24 subjects were included in the final study population: 19 men and five women, with a mean age of 60 years (± 12.3 years). Eight patients were eliminated due to excessive head motion, technical failure, or incomplete acquisition of fMRI data.
Two of the study's researchers conducted the image analysis, which included calculating stroke lesion volume, the extent of white-matter lesions, and regional cerebral blood flow in core areas of the default mode network. To measure fMRI activity, the group developed a functional connectivity index based on the time series of voxels in the default mode network area of the brain.
At the three-month follow-up, 14 patients had no signs of depression, while 10 individuals were diagnosed with minor to moderate depression. There was a significant correlation between the HDRS 17 and HARS scores at the three-month mark, the authors wrote.
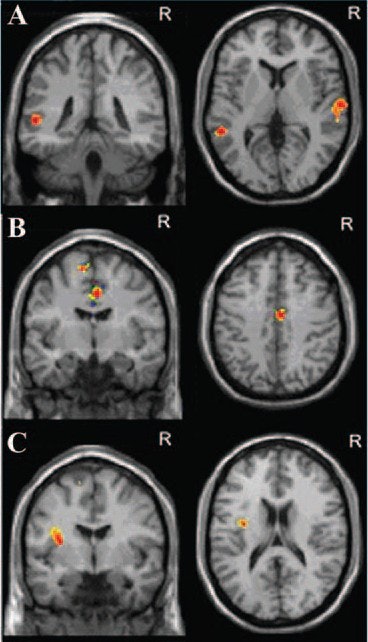 |
| Axial and coronal MR images show correlation between default mode network functional connectivity and severity of early anxiety symptoms. Anxiety symptom severity measured at 10-day follow-up correlates positively with functional connectivity index in (A) left and right middle temporal cortices and correlates negatively with (B) anterior midcingulate cortex and (C) left insula. Images courtesy of Radiology. |
Finding connections
The authors attempted to correlate depression severity on the HDRS 17 and HARS scales with functional activity in various brain areas at different follow-up times on fMRI.
With respect to early mood symptoms, the researchers found no correlation between HDRS 17 depression score and the functional connectivity index at the 10-day follow-up point. However, they found that the HARS score for anxiety correlated positively with the rest functional connectivity index of the right and left middle temporal cortex.
Regarding late mood symptoms at the three-month follow-up, the left middle temporal cortex rest functional connectivity index correlated positively with both the HDRS 17 and HARS scales.
"These results support a strong association between early resting-state network impairments and the risk of poststroke mood disorders," the authors wrote. "We found a strong association between [the middle temporal cortex] functional connectivity and mood symptom severity at early and late poststroke phases."
The middle temporal cortex is involved in the perception of negative emotional facial expressions and affective empathy and is considered part of a network involved in the comprehension of others' mental states, they noted.
Sibon and colleagues acknowledged that the findings should be interpreted "with caution" due to several limitations of the study. One such limitation is the exclusion of patients with severe physical impairment, which limits the degree to which the results can be generalized to other groups.




















