The Medical Imaging and Technology Alliance (MITA) is criticizing the U.S. Centers for Medicare and Medicaid Services' (CMS) inpatient prospective payment system (IPPS) final rule.
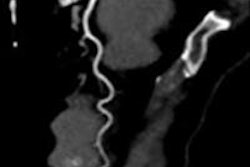
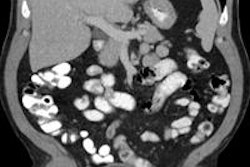
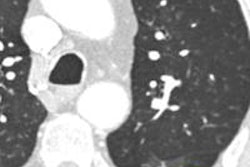
Issued on August 2, the rule changes CMS reimbursement for the technical component of hospital inpatient imaging by establishing separate cost estimates, or cost-to-charge centers, for CT and MRI exams. Opponents of the rule believe that it could lead to dramatically lower reimbursement for CT and MRI scans.
MITA believes the IPPS rule is based on inaccurate payment models and will jeopardize patient access to CT and MR services. Under the policy, CMS pays hospitals nearly the same rate for advanced CT as it does for x-ray, Gail Rodriguez, MITA's executive director, said in a statement.
CT and MRI services are capital-intensive and allocation of capital costs within the cost reports is both complicated and subject to error, according to the organization. The new CT and MR cost centers employed in the final rule result in payment rates that do not reflect the differences in diagnostic power between imaging tests, as well as a hospital's investment in advanced imaging technology, MITA said.
Furthermore, CMS is currently proposing to use the same cost model to determine hospital outpatient payments. CMS' own analyses show that payments will drop by as much as 38% for CT and 19% for MR when it is applied to the outpatient setting, MITA said.