Egyptian researchers found that CT-guided percutaneous needle biopsy (PCNB) is accurate and effective for diagnosing lesions of the appendicular long bones -- offering a much-needed solution to the problem of indeterminate x-rays, according to an article in the European Journal of Radiology.
Assessing results of the technique in 49 patients, the study team found an overall diagnostic yield of 88% with at initial biopsy compared with surgical results as the gold standard. Higher performance was obtained for malignancies, lesions with an extraosseous tissue component, and those with mixed and sclerotic lesions. Less accurate were diagnoses of large-cell lymphoma, giant-cell tumors, and osteoid sarcomas, among other findings.
"Our study concludes a high diagnostic performance of initial CT-guided PCNB in extremity long bone lesions especially in the settings of malignant, mixed, and/or sclerotic lesions as well as extraosseous exophytic tissue growth," wrote Dr. Mohamed Ragab Nouh from Alexandria University, Egypt, and Dr. Hamdy Mohamed Abu Shady from al-Razi hospital in Sulibikhate, Kuwait. "On the other hand, there were some inherent limitations in benign and/or cystic lesions, where assessment of tissue architecture is essential for proper pathologic diagnosis" (Eur J Radiol, 27 October 2013).
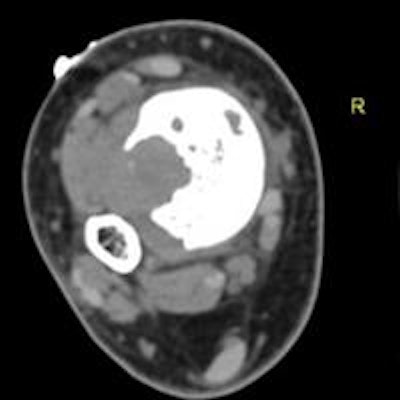
 A 15-year-old boy presented with a metaphyseal lucent lesion with well-defined borders that remained quiescent for two years. The patient recently complained of persistent pain and progressive appearance of right ankle swelling. X-ray showed complete changes of the lesion's behavior into a punched-out defect of the distal tibial metadiaphyseal lesion with violated cortex and indeterminate zone of transition, no periosteal reaction or matrix formation were identified. The differential included ruptured chronic bone abscess, Langerhans cell histiocytosis (LCH), and marrow neoplasia. CT-guided biopsy was planned through the large exophytic soft-tissue component seen on CT. This allowed harvesting multiple cores from the main lesion within the bone. The biopsy returned with the result of fibroblastic osteosarcoma. Above, x-ray distal both leg bones and ankle in anteroposterior (left image) and lateral (right image) projections showing distal tibial metadiaphyseal cortical and eccentric lesion with cortical defect and indeterminate medial margin. Neither periosteal reaction nor matrix formations are recognized. Below, axial CT scans of the distal tibial lesion in soft-tissue window setting prior to start of the CT-guided procedure (left image) and bone window setting during the procedure (image at right). All images courtesy of Dr. Mohamed Ragab Nouh.
A 15-year-old boy presented with a metaphyseal lucent lesion with well-defined borders that remained quiescent for two years. The patient recently complained of persistent pain and progressive appearance of right ankle swelling. X-ray showed complete changes of the lesion's behavior into a punched-out defect of the distal tibial metadiaphyseal lesion with violated cortex and indeterminate zone of transition, no periosteal reaction or matrix formation were identified. The differential included ruptured chronic bone abscess, Langerhans cell histiocytosis (LCH), and marrow neoplasia. CT-guided biopsy was planned through the large exophytic soft-tissue component seen on CT. This allowed harvesting multiple cores from the main lesion within the bone. The biopsy returned with the result of fibroblastic osteosarcoma. Above, x-ray distal both leg bones and ankle in anteroposterior (left image) and lateral (right image) projections showing distal tibial metadiaphyseal cortical and eccentric lesion with cortical defect and indeterminate medial margin. Neither periosteal reaction nor matrix formations are recognized. Below, axial CT scans of the distal tibial lesion in soft-tissue window setting prior to start of the CT-guided procedure (left image) and bone window setting during the procedure (image at right). All images courtesy of Dr. Mohamed Ragab Nouh.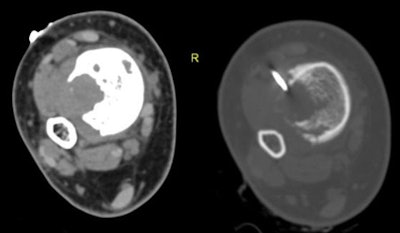
In an email to AuntMinnieEurope.com, Nouh said the real value of the study is that it "clarifies that adherence to the old school interdisciplinary algorithmic approach to such lesions will help the radiologist, as well as physician in charge to optimize patient management."
These results are accomplished by incorporating:
- Meticulous assessment of the patient's history and assessment of the presenting clinical setting
- Revision of all available imaging studies to better characterize the lesion and hosting bone
- Assessing whether CT-guided percutaneous biopsy will be of benefit for the case in discussion or it is preferable to go directly for open surgical biopsy to minimize any delay in patient treatment
Long bones a common target for lesions
The appendicular long bones host a wide range of bony lesions, as well as osteomyelitis, reactive focal abnormalities, and tumor-like lesions. Bony lesions often present as pain, swelling, and pathologic fractures.
And unfortunately, advances in diagnostic imaging techniques have not solved the problem of diagnosing bony lesions, which are difficult to assess on radiography, even though it is the modality that detects the majority of them, according to the authors.
Most previous studies didn't distinguish between initial versus repeat biopsy procedures, and included soft-tissue lesions in addition to bony lesions leading to a measure of artificial inflation of the accuracy, the authors wrote. Therefore, this study aimed to assess the diagnostic performance of initial CT-guided needle biopsies of extremity long bone lesions at a tertiary musculoskeletal referral center.
The study team looked at results in 49 patients who underwent the procedure between 2010 and 2012.
They made the decision to perform a biopsy in an interdisciplinary manner between an orthopedic surgeon and musculoskeletal radiologist, choosing the biopsy instrumentation and sampling site individually for each patient.
Included were patients with pathologic fractures, incidentally detected bony lesions suspected of being sarcomas, or metastases. Excluded were patients with lesions confined to the soft tissues. The authors probed patient records to assess demographics, history, and management strategies, as well as the results of previous imaging and biopsies.
In all, 49 patients including 23 men and 15 women (mean age 33.7 years, range 4-77 years) underwent image-guided biopsies. Imaging in the cohort included radiography, CT, and MRI, and the study team categorized the records according to the location of the host bone, presence or absence of an extraosseous soft-tissue component (usually at MRI), and imaging nature of the lesion matrix (usually at CT) including lytic, sclerotic, or mixed lytic and sclerotic.
After bleeding, the researchers collected procedure parameters and lab markers. An experienced musculoskeletal radiologist performed all biopsies under CT guidance, with most patients in a state of conscious sedation so they could lie down comfortably, the authors wrote.
Initial biopsies revealed an overall diagnostic yield of 87.75% (43 of 49 cases), and diagnostic accuracy 82.85% based on surgically proven cases. The authors found no biopsy-related complications such as hematoma or infection. Six cases were nondiagnostic; in five because the sample contained hemorrhagic components, necrotic tissues, or tissues with a large portion of fibrous elements, the study team wrote.
In these six cases they "considered the specimen inadequate to provide specific tissue diagnosis and recommended a larger tissue core from a surgical specimen," the authors wrote. These cases were finally diagnosed as: large-cell lymphoma, giant-cell tumor, langerhans cell histiocytosis, osteoid osteoma, and a nonossifying fibroma. In the remaining case, a tibial lesion was diagnosed as fibrous dysplasia following CT-guided percutaneous biopsy, which proved to be adamantinoma on the postsurgical pathology report.
Cross-sectional imaging showed an extraosseous component in about half (26/49) patients, which facilitated biopsy and obviated the need for cortical breach, the authors wrote. The other 23 patients had completely intraosseous lesions that required more aggressive efforts to reach the lesion, the study team wrote.
The femur was the most common bone biopsied at 37% of cases, followed by the humerus at 29%, and the tibia at 22%.
The highest initial diagnostic yields were recorded in the humerus and fibula; the lowest diagnostic yields were in the radius. Percutaneous biopsy confirmed all six cases of metastatic bony lesions, and biopsy yielded the correct diagnosis in two-thirds of hematologic malignancies, 29/32 cases of primary malignant bone tumors, and 10/12 nonmalignant bone processes.
Based on imaging findings at CT and x-ray, initial diagnostic yield was higher for mixed lesions (94%), followed by sclerotic (89%) and lytic (83%) lesions, according to the authors. As for the completely intraosseous lesions, the diagnostic yield was 74%, while the presence of extraosseous soft-tissue components raised the diagnostic yield to 100% in 26 cases.
Higher diagnostic yields were found in cases of malignancy, with the presence of extraosseous soft-tissue component, and in mixed and sclerotic lesions.
The pathologies of the six nondiagnostic biopsies included large-cell lymphoma, giant-cell tumor, langerhans cell histiocytosis, osteoid osteoma, and a nonossifying fibroma. Initial biopsy successfully diagnosed 2/3 of cases with hematologic malignancies, 29/32 primary malignant bone tumors, and 10/12 nonmalignant bone processes, the group wrote.
"The image-guided percutaneous biopsy has proved to be a safe, minimally invasive, and cost-effective procedure for the diagnosis of skeletal lesions, obviating the need for the more risky and invasive open surgical biopsy in most patients, wrote Nouh and Abu Shady. "Meticulous technique regarding compartmental barriers, neurovascular structures, and seeding of malignant cells along the biopsy needle track are prerequisites for optimized treatment strategies with limb-salvage procedures. CT has proven to be a recognized modality for guiding PCNB of deep-seated musculoskeletal lesions."
Potential complications include pain, hematoma, infection, and potential tumor seeding along the needle path -- however a recent report found the risk of this complication to be negligible. And no complications from biopsy were seen in the study population.
Diagnostic accuracy of 82.85% for the nonsurgically proven cases compares well with the results of percutaneous musculoskeletal biopsies of falling in the range of 69% to 98% from different musculoskeletal regions. But while many of the cases in that study were diagnosed in the second biopsy try, the present study relied solely on the results of first biopsies, the group noted. Yet the high diagnostic yield of metastatic and primary malignancies is in line with previous studies. The success might be attributed to the compact nature of malignant neoplasm's cells, the team wrote.
"In the current study, the nondiagnostic cases varied between benign lesions (osteoid osteoma and nonossifying fibroma), low-grade malignancies (adamantinoma and giant cell tumor), systemic hematologic malignancy (large-cell lymphoma), and the indeterminate entity of Langerhans cell histiocytosis," the group wrote. Their pathologic reports described the presence of fibrous tissue, necrosis, or blood. Likewise, similar tissue compositions were associated with false negative results in previous works."
Several causes of the low diagnostic yields in these lesions could be at play, the team noted. First, benign mesenchymal lesions have a dominant architecture of a few loose cells "in abundant loose stroma" necessitating a large sample size, they wrote. Second, low grade tumors like giant-cell tumors and andadmantinoma consist of heterogenic cells with nonconsistent morphology. Similarly, hematologic tumors are formed of loose tissues, some of which may be necrotic. And all nondiagnostic tumors were completely intraosseous lesions, which inhibits the tissue sample rate, they wrote.
The lesion matrix, as visualized on the different imaging modalities, is a major factor determining the biopsy instrumentation choice and percutaneous biopsy decision, the authors wrote. In line with previous studies, the study reached higher diagnostic yields for lesions of mixed matrices, followed by sclerotic lesions and lytic lesions.
"We found that lesions with extraskeletal soft-tissue components or intraosseous lesions with rarified cortices over them scored well in our study," Nouh wrote in his email. "Also, mixed lytic and sclerotic lesions yielded good results compared to the lytic lesions.
The more aggressive appearance of the lesion on imaging resulted in high diagnostic yield. This might be due to variability of cellular elements in the biopsied tissues as well as their compactness."
The study was limited by its retrospective design, small sample size, and the participation of multiple pathologists with varying experience levels, they noted.
The authors also cited close collaboration between an orthopedic surgeon and radiologist as instrumental in achieving a high diagnostic rate in lytic and sclerotic lesions.
The careful and interdisciplinary approach to determining biopsy targets avoids "unnecessary biopsies for the common group of 'leave me alone' lesions and minimizes the need for biopsying such lesions in a patient with a known primary with tendency for skeletal metastatic disease e.g. the common breast and prostatic neoplasias," Nouh told AuntMinnieEurope.com.
Finally, the authors emphasized the importance of managing patients in a tertiary musculoskeletal center with an interdisciplinary team approach to achieve the best outcomes.