The use of PET/CT with a sodium fluoride (NaF) radiopharmaceutical produces high sensitivity, suggesting that the modality can be beneficial in detecting bone metastases caused by prostate cancer, according to a study published in the November issue of the American Journal of Roentgenology.
In a comparison with diffusion-weighted MRI (DWI-MRI), Swedish researchers found that NaF-PET/CT achieved greater sensitivity, while DWI-MRI achieved greater specificity in discovering bone metastases. The study's findings offer evidence that both modalities may be more efficient than bone scintigraphy, which traditionally has been the modality of choice to detect bone metastases in high-risk prostate cancer patients.
While bone scintigraphy has been used for several decades, the modality can result in false-positive findings in degenerative changes, inflammation, and trauma. "New methods with higher accuracy are worth discussing because the suboptimal specificity and sensitivity of bone scintigraphy are concerning," wrote lead author Dr. Firas Mosavi, from the department of radiology at Uppsala University Hospital, and colleagues (AJR, November 2012, Vol. 199:5, pp. 1114-1120).
Past studies have shown that DWI-MRI provides functional information based on water molecule motion, according to the authors; solid tumors are detected through restricted diffusion due to high cellular density. Sodium fluoride is a highly sensitive and specific bone imaging agent, which previous studies have shown can be more effective in detecting bone metastases than bone scintigraphy.
The prospective study analyzed 49 consecutive patients with newly diagnosed prostate cancer. All subjects underwent bone scintigraphy, whole-body MRI, and NaF-PET/CT to detect bone metastases between October 2009 and March 2011. The median age of the patients was 67 years, ranging from 57 to 80 years.
Participants were included in the study if their biopsy positively diagnosed prostate cancer. The researchers excluded patients who had a history of a second cancer and who could not undergo an MRI scan for reasons such as claustrophobia, metal implants, or pacemakers.
Patients with bone lesions who were strongly suspected of having metastases at the time of diagnosis were monitored with at least one of the initially performed modalities. The longest time of follow-up imaging was 14 months. Clinical and laboratory follow-up were arranged for all patients, ranging from seven to 24 months.
Imaging protocol
NaF-PET/CT imaging (Discovery ST, GE Healthcare) was conducted one hour after patients received 3 MBq/kg body weight of NaF. Images were acquired from the vertex to one-third down the thigh, with an acquisition time of two minutes per bed position in 3D mode. DWI-MRI was performed on a 1.5-tesla MRI system (Gyroscan Intera, Philips Healthcare) with a whole-body built-in coil.
Whole-body bone scintigraphy scans were performed using a dual-head gamma camera (Infinia Hawkeye, GE) three hours after injection of 600 MBq of hydroxymethylene diphosphonate labeled with technetium-99m. Bone scintigraphy, conventional MRI, and follow-up images were used as a standard of reference to evaluate NaF-PET/CT and DWI results.
The median time between the three imaging exams was seven days, ranging from two to 48 days, and all imaging procedures were performed before participants began therapy. Readers who interpreted the images were blinded to all clinical data except in cases of patients diagnosed with high-risk prostate cancer.
The most common sites for metastases were in the pelvis and spine, and there were no other metastases outside of those locations, the researchers found. The patient-based analysis revealed that 16 (33%) of the 49 patients had at least one metastasis found by one of the three imaging modalities. Only five patients (9%) had skeletal metastases that were verified by both DWI-MRI and NaF-PET/CT.
Of those five patients, two had widespread bone metastases and died eight and 16 months after the initial imaging. The other three subjects showed partial regression on follow-up studies.
NaF-PET/CT detected more true-positive lesions in four of five patients with bone metastases compared to DWI-MRI, and it detected an equal number of lesions in the fifth patient.
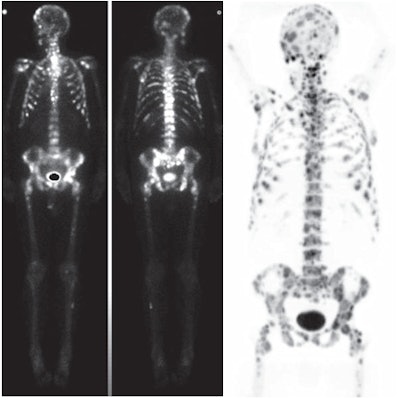 |
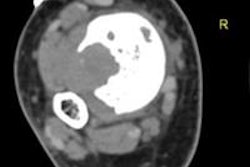
| Numerous bone metastases were detected in a 67-year-old man with prostate cancer. Bone scintigraphy (left) and NaF-PET/CT (right) images show more lesions in skull and ribs than whole-body bone MRI. Images courtesy of the American Journal of Roentgenology. |
There were no false-negative results with either of the two modalities, whereas NaF-PET/CT showed false-positive results in four patients and DWI-MRI had one false-positive finding. In addition, there were no signs of metastases in 40 patients (81%) with NaF-PET/CT, compared with 43 patients (86%) with DWI. Results from these patients were true-negative findings.
In the lesion-based analysis, NaF-PET/CT detected nine true-positive lesions, compared with five true-positive lesions with DWI-MRI. There were no false-negative results with NaF-PET/CT, compared with four false-negative lesions at DWI, and there were seven false-positive findings with NaF-PET/CT, compared with two false-positive results at DWI.
Two patients with uncountable bone metastases were analyzed separately. In these patients, NaF-PET/CT showed more bone metastases than DWI-MRI.
Additional research
"Our prospective study results suggest that NaF-PET/CT has higher sensitivity but lower specificity than whole-body DWI for detection of bone metastases from prostate cancer," the authors concluded.
They noted that the lesions in the study were compared with a radiologic reference standard and follow-up studies, and no biopsies were performed.
"In clinical practice, NaF-PET/CT is a new imaging method," they added. "The lack of previous clinical experience in interpretation of this imaging modality has probably led, to some extent, to a high amount of false-positive findings."
More studies with larger patient populations should be conducted to confirm the results before clinical adoption of these methods can be endorsed, the group wrote.