Researchers using automated software to assess bone scintigraphy scans of patients with metastatic prostate cancer found that the algorithm helped them predict which patients were more likely to survive, compared with manual methods of interpreting the scans, according to a May 17 paper in JAMA Oncology.
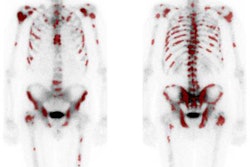
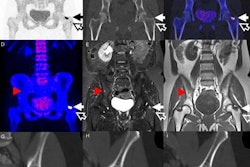
Bone scintigraphy with technetium-99m (Tc-99m) is the standard modality for detecting whether cancer has spread to the bone in men with metastatic castration-resistant prostate cancer. But existing methods for analyzing the scans rely on manual interpretation, such as by counting the number of metastatic lesions; this can cause variability due to subjective interpretation, according to the research team, which was led by Dr. James Armstrong of Duke University (JAMA Oncol, May 17, 2018).
A software application has been developed (automated bone scan index or aBSI; Exini Diagnostics) that uses artificial neural networks to detect and classify "hot spots" in bone scintigraphy scans. The application then produces an automated bone scan index that represents the total tumor burden in the patient as a percentage of his weight.
Armstrong and colleagues tested the software in a randomized trial of men being seen at 241 sites in 37 countries from 2011 to 2015 as part of a phase III trial of the tasquinimod therapeutic agent. A total of 721 men were found to be eligible for the BSI arm of the study.
The aBSI scores calculated by the software were associated with the study's primary end point, death, as well as other end points including prostate cancer-specific survival, radiographic progression-free survival, time to symptom progression, and time to opiate use for cancer pain.
For the entire patient population, the median aBSI score was 1.07, with a range of 0 to 32.6. Patients were divided into quartiles based on their scores: The lowest scores were in quartile 1 (indicating the lowest lesion burden) and the highest were in quartile 4. Outcomes were then analyzed by quartile.
The risk of death from any cause increased by 20% for every doubling of the aBSI score, the researchers found. Scores by quartile are shown in the following table, compared with those in quartile 4 (the highest lesion burden).
| Reduction in risk of death by aBSI score quartile, compared with quartile 4 | |||
| Quartile 3 | Quartile 2 | Quartile 1 | |
| Reduction in risk of death | 40% | 56% | 65% |
Armstrong and colleagues also found correlations between aBSI scores and other outcome measures, leading the group to conclude that automated scoring of bone scintigraphy studies with the software was an accurate tool for predicting survival in patients with metastatic castration-resistant prostate cancer.
"The aBSI provides a rapid quantitative measure of bone burden with clear prognostic utility and is strongly associated with time to new bone metastases, time to symptomatic progression, and time to opiate use for cancer pain," they wrote.
They further concluded that aBSI scores could be used to guide therapy in these patients.