Challenges remain on the road to more precise assessment of tumor treatment response with CT perfusion (CTP), but the techniques are already robust and far more sensitive than the old methods based on tumor size. In this emerging field, tumor biology and treatment response combine to make CT an ideal modality for monitoring cancer treatment, according to Boston researchers.
In a discussion of the successes and possibilities of CT perfusion in oncology, Dr. Dushyant Sahani spoke of broad efforts to develop biomarkers to assist in various stages of cancer care, from risk assessment to early detection, treatment selection, and assessment of response for early intervention.
"We have seen tremendous evolution in the treatment methods available for oncologic patients; we have organ-directed therapies, ablative techniques, intra-arterial techniques, and even targeted radiotherapies which are often given with image guidance," said Sahani, who is a professor of radiology at Harvard Medical School and a radiologist at Massachusetts General Hospital.
 Dr. Dushyant Sahani from Harvard Medical School and Massachusetts General Hospital.
Dr. Dushyant Sahani from Harvard Medical School and Massachusetts General Hospital.Most important are the new molecularly targeted drugs, which don't necessarily cause cell death but decrease vascularity or cell proliferation through various tumor targets, he said in a talk at the International Symposium on Multidetector-Row CT (MDCT 2014) in San Francisco in June.
Targeted therapies
Advances in cancer biology and cytogenetics have produced targeted biologic cancer therapies that work on cell membrane receptors. Examples include vascular endothelial growth factor receptors (VEGFRs), epidermal growth factor receptors (EGFRs), and platelet-derived growth factor receptors (PDGFRs).
Radiologists may not be used to seeing the effects of the various treatments on CT images, but the therapies are ideal for CT perfusion because most target blood flow, and contrast enhancement has a linear relationship with contrast at CTP, Sahani said.
The conventional way of evaluating treatment response is to look for changes in tumor burden over time as manifested in diameter or volume. But the new drugs don't necessarily change tumor size -- rather, they target its viability, often by affecting blood flow.
"A tumor causes changes in vascularity due to neoangiogenesis and changes in contrast media kinetics, so if we can do dynamic imaging and apply kinetic modeling, we can estimate the changes in physiologic parameters due to changes in microvasculature in the tissue," Sahani explained.
Such calculations are possible for CT because changes in attenuation have a linear relationship with the amount of iodine present, enabling mathematical modeling of the treatment response based on attenuation.
Perfusion CT is typically performed using a low mA setting and a small amount of contrast media that is injected quickly to achieve strong peak arterial enhancement, Sahani said. Then, mathematical modeling of CT images based on perfusion software yields a range of parameters, including the following:
- Regional blood flow
- Regional blood volume
- Mean transit time
- Permeability surface area product
- Time to peak enhancement
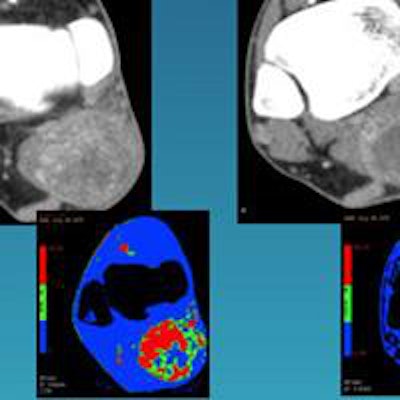
CT perfusion images can be processed to provide a visual map, or the parameters can be quantified to demonstrate the changes occurring on a microvascular level, changes that tend to occur in predictable ways depending on the treatment.
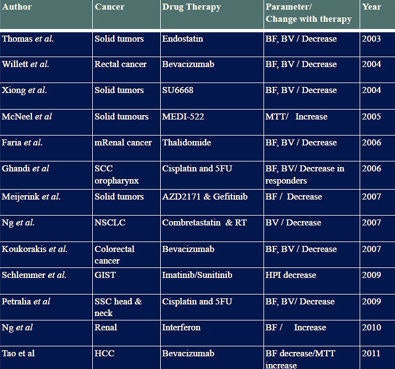
For example, at the MDCT 2013 meeting, Dr. Vicky Goh, chair of clinical cancer imaging at King's College London and a radiologist at Guy's and St. Thomas' Hospitals National Health Service Foundation, showed the anticipated effects of a range of treatments. For example, chemotherapy could be expected to reduce regional blood volume, blood flow, and extraction fraction, while radiation boosts and then reduces the same parameters, Sahani said.
In the setting of colorectal cancer, treatment with the antiangiogenic drug bevacizumab (Avastin, Genentech/Roche), for example, produced more than a 50% drop in tumor vascularity on perfusion CT, which did not occur in PET imaging, Sahani said of a 2011 study by Willett et al. By the end of treatment, the changes in CT perfusion and PET were both pretty substantial, but CT found the treatment response first.
"These dynamic [CTP] images are the most sensitive way to look at microvascular changes," he said. "We saw a similar effect in hepatic carcinomas, which tend to be angiogenic."
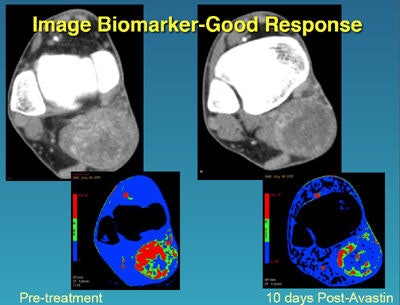 In a sarcoma patient, images before treatment and 10 days later show the treatment is working and should be continued. All images courtesy of Dr. Dushyant Sahani.
In a sarcoma patient, images before treatment and 10 days later show the treatment is working and should be continued. All images courtesy of Dr. Dushyant Sahani.In one hepatocellular carcinoma (HCC) patient, the drop in vascularity was nearly 90% after two weeks of treatment, solid evidence that a combination of gemcitabine, oxaliplatin, and bevacizumab was working.
In HCC treatment, they also noticed that if certain perfusion parameters such as mean transit time were higher at baseline, those tumors showed better response and progression-free survival. "So some of these parameters might have prognostic value of response," Sahani said.
In the past decade, dozens of studies using novel targeted therapies have demonstrated tumor treatment response on perfusion CT, he said. And studies to date have shown that early treatment response can often determine prognosis.
Challenges remain
Still, to say everything wraps up neatly at that point would be false, as several challenges associated with CTP for monitoring individualized treatment response remain. Treatment assessment with CT perfusion is not as advanced as it should be, according to Sahani.
"One reason perfusion CT is not as popular as it could be is the availability and expertise needed to apply the techniques," he said. "Standardization of protocols is essential as there are different kinds of scanners and techniques -- and as of now no multicenter trials."
 Dozens of studies over the past several years have used CTP to measure treatment response. But the field suffers from a lack of experienced radiologists, multicenter trials, and validated protocols.
Dozens of studies over the past several years have used CTP to measure treatment response. But the field suffers from a lack of experienced radiologists, multicenter trials, and validated protocols.Robust and reliable analysis is required for accuracy and reproducibility of CTP techniques. How the region of interest is selected and how the CT values are compiled (averaged data or voxel by voxel) can have important effects, as can the software that is used to analyze the data. At least a multicenter trial is on the way, Sahani said.
"But despite the limitations, I think there is a lot of promise in perfusion imaging," he said. "It's worth investing the time and effort to look at CT along with conventional ways of tumor staging and also functional assessment, but it requires some work for implementation in a clinical trial."